Introduction
Physiotherapy in Kitchener for Knee
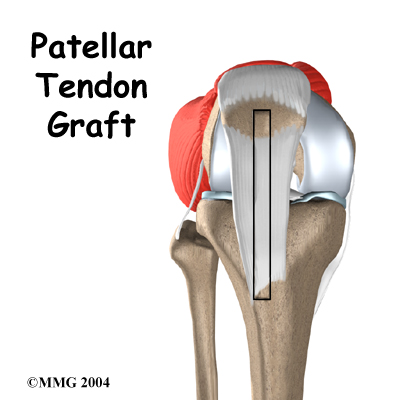
Welcome to Kitchener Physiotherapy & Wellness patient resource about Patellar Tendon Graft Reconstruction of the ACL.
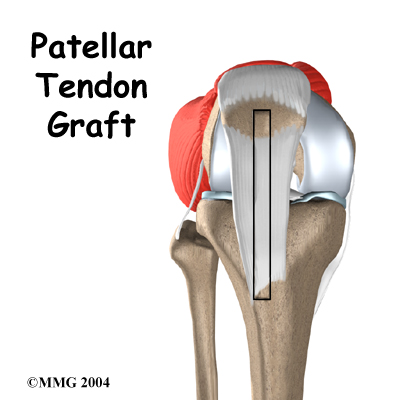
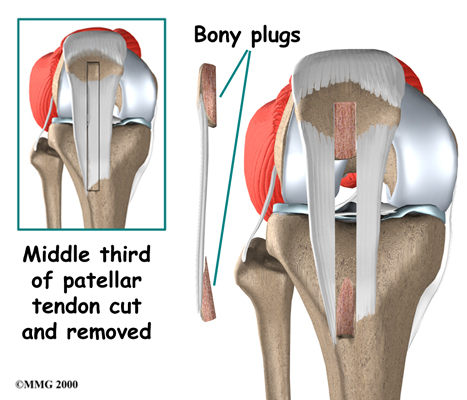
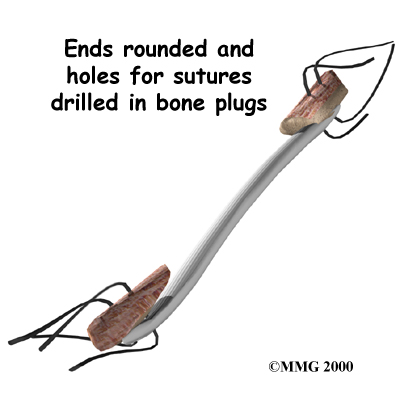
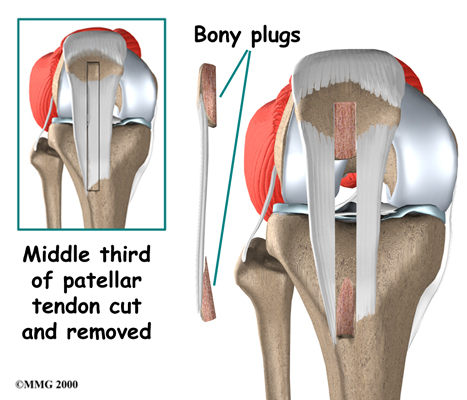
The anterior cruciate ligament (ACL) is a major stabilizer of the knee joint. This key knee ligament is commonly torn during sports activities. The standard operation to fix a torn ACL is with a patellar tendon graft. The surgeon takes out the middle section of the patellar tendon below the kneecap (patella). This new graft includes the strip of tendon, along with attached plugs of bone on each end. For this reason, it is sometimes referred to as a bone-patellar-tendon-bone graft. The surgeon removes the torn ACL and puts the new graft into the knee, making sure to line it up just like the original ligament.
Many types of tissue grafts have been tried. The patellar tendon graft has proven to be one of the strongest for ACL reconstruction. Patients who have this operation generally get back to their usual activities and sports. They often do so faster than people who have their ACL reconstructed with other types of tissue grafts.
This article will help you understand:
- what parts of the knee are treated during surgery
- how surgeons perform the operation
- what to expect before and after the procedure
Related Document: Kitchener Physiotherapy & Wellness Guide to Anterior Cruciate Ligament Injuries
Anatomy
What parts of the knee are involved?
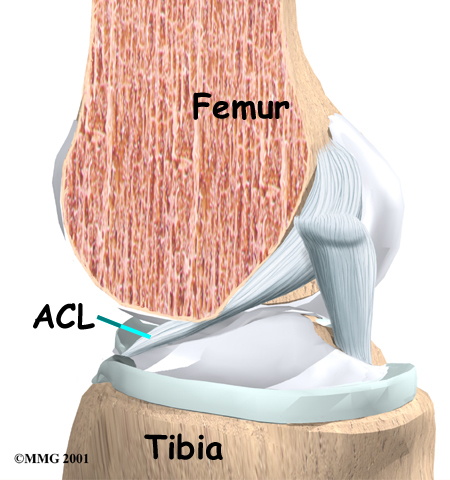
Ligaments are tough bands of tissue that connect the ends of bones together. The is located in the center of the knee joint where it runs from the backside of the femur (thighbone) to the front of the tibia (shinbone).
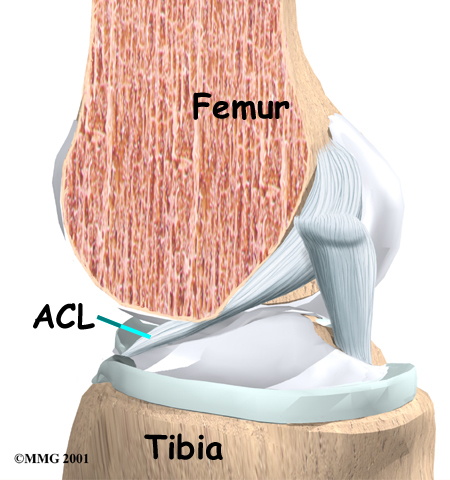
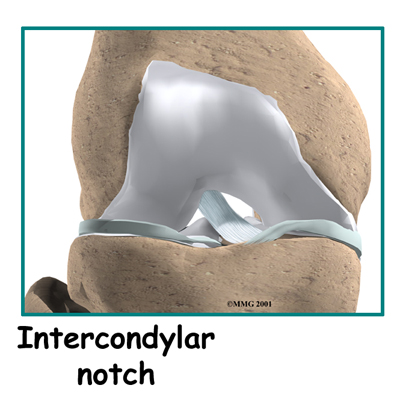
The ACL runs through a special notch in the femur called the and attaches to a special area of the tibia called the tibial spine.
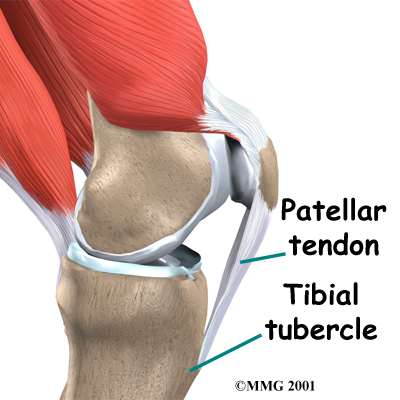
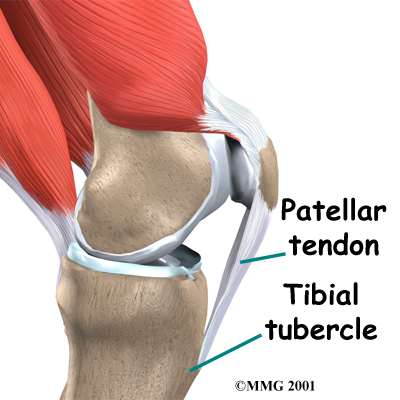
The is a thick and strong band of connective tissue on the front of the knee. It starts at the bottom of the patella and fastens just below the knee to a bony bump on the front of the tibia, called the tibial tubercle. When using the patellar tendon as an ACL graft, surgeons remove a strip from the middle of it. The graft includes the bony attachments from the bottom of the patella and from the tibial tubercle.
Related Document: Kitchener Physiotherapy & Wellness Guide to Knee Anatomy
Knee Anatomy Introduction
Rationale
 What does the surgeon hope to accomplish?
What does the surgeon hope to accomplish?
The main goal of ACL surgery is to keep the tibia from moving too far forward under the femur bone and to get the knee functioning normally again.
Many surgeons prefer to use the patellar tendon when reconstructing the ACL. The graft is often chosen because it is one of the strongest ACL grafts. It's easy to get to, holds well in its location, and generally heals fast.
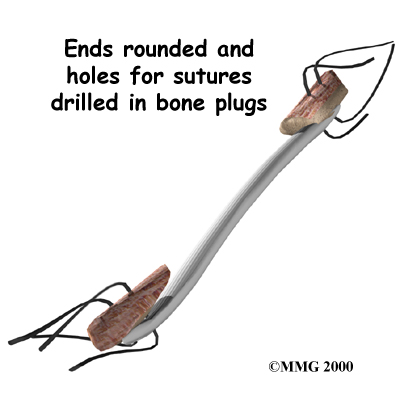
The anatomy of the graft helps to speed healing and to create a solid connection. When the surgeon implants the new graft, the on each end of the graft fit inside a tunnel of bone. This means there is bone-to-bone contact. The body treats the contact of these two bony surfaces as it would a broken bone. It responds by healing the two surfaces together. Healing at the bone-to-bone surface fixes the patellar tendon graft in place.
Preparation
What do I need to know before surgery?
You and your surgeon should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physiotherapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this preoperative visit is to record a baseline of information. Your therapist will check your current pain levels, your ability to do your activities, and the movement and strength of each knee.
A second purpose of the preoperative visit is to prepare you for surgery. Your therapist will teach you how to walk safely using crutches or a walker. And you'll begin learning some of the exercises you'll use during your recovery.
On the day of your surgery, you will probably be admitted to the surgery center early in the morning. You shouldn't eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
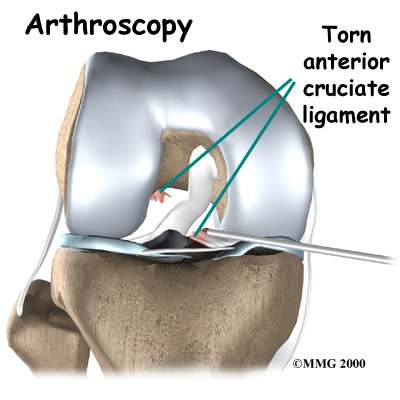 Most surgeons perform this surgery using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during for this procedure. The operation doesn't require the surgeon to open the knee joint.
Most surgeons perform this surgery using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during for this procedure. The operation doesn't require the surgeon to open the knee joint.
Before surgery you will be placed under either general anesthesia or a type of spinal anesthesia.
The surgeon begins the operation by making two small openings into the knee, called portals. These portals are where the arthroscope and surgical tools are placed into the knee.
Care is taken to protect the nearby nerves and blood vessels.
A small incision is also made below the patella. Working through this incision, the surgeon takes out the middle section of the patellar tendon, along with the bone attachments on each end. The are rounded and smoothed. Holes are drilled in each bone plug to place sutures (strong stitches) that will pull the graft into place.
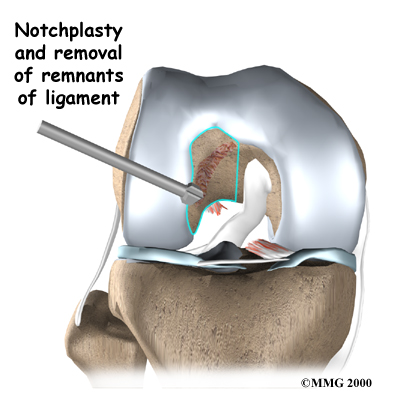
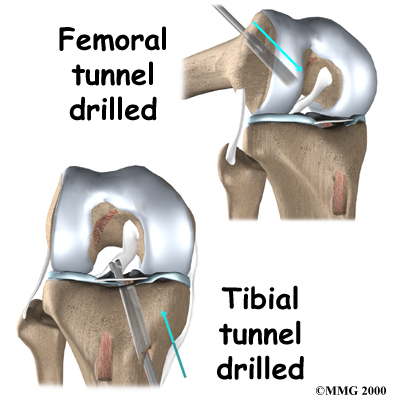
Next, the surgeon prepares the knee to place the graft. The remnants of the original ligament are removed. The intercondylar notch (mentioned earlier) is enlarged so that nothing will rub on the graft. This part of the surgery is referred to as a:
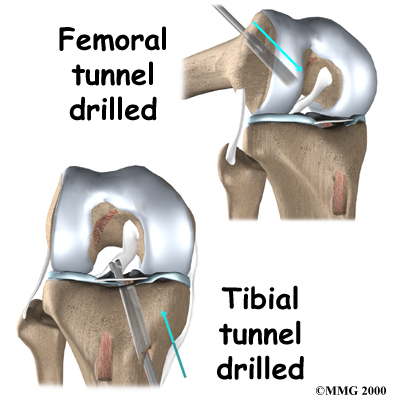
Once this is done, in the tibia and the femur to place the graft. These holes are placed so that the graft will run between the tibia and femur in the same direction as the original ACL.
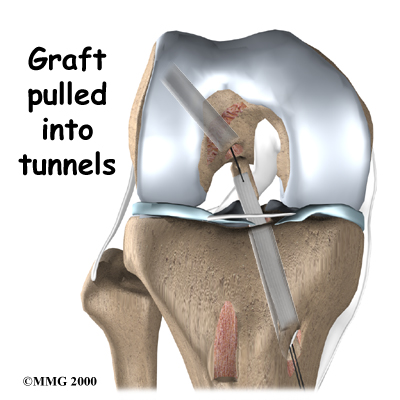
The graft is then using sutures placed through the drill holes. Screws are used to hold the bone plugs in the drill holes.
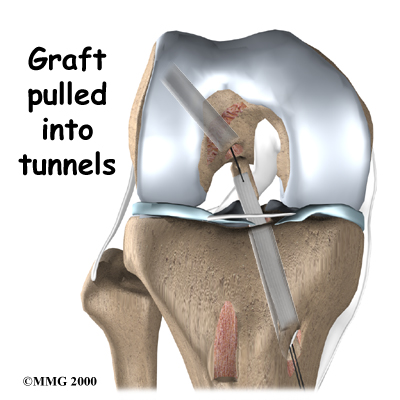
To keep fluid from building up in your knee, the surgeon may place a tube in your knee joint. The portals and skin incision are then stitched together, completing the surgery.
Complications
What problems can happen with this surgery?
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following patellar tendon graft reconstruction of the ACL are:
- anesthesia complications
- thrombophlebitis
- infection
- problems with the graft
- problems at the donor site
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include:
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following surgery, it is possible that the surgical incision can become infected. This will require antibiotics and possibly another surgical procedure to drain the infection.
Problems with the Graft
After surgery, the body attempts to develop a network of blood vessels in the new graft. This process, called revascularization, takes about 12 weeks. The graft is weakest during this time, which means it has a greater chance of stretching or rupturing. A stretched or torn graft can occur if you push yourself too hard during this period of recovery. When revascularization is complete, strength in the graft gradually builds. A second surgery may be needed to replace the graft if it is stretched or torn.
Problems at the Donor Site
Problems can occur at the donor site (the area below the patella where the graft was taken from the knee). A major drawback of taking out a piece of the patellar tendon to reconstruct the ACL is that most patients end up having difficulty kneeling down long after surgery. Lingering pain in the front of the knee is also common.
A portion of bone is taken from the bottom of the patella during the graft procedure. This can weaken the patella. In rare cases, heavy use of the quadriceps muscle (on the front of the thigh) can cause the patella to fracture. This often requires a second surgery to repair the broken patella.
Taking tissue from the center of the patellar tendon can also cause problems. The body attempts to heal the area but sometimes produces too much scar tissue. The extra scar tissue that forms around the donor site may prevent normal motion in the knee. The patellar tendon is not as strong as it was before surgery. In rare cases, this has been linked to a tear in the patellar tendon. Also, the patellar tendon may become easily inflamed. And problems in this area can keep the quadriceps from regaining normal control and strength.
After Surgery
What should I expect after surgery?
You may use a continuous passive motion (CPM) machine immediately afterward to help the knee begin moving and to alleviate joint stiffness. The machine straps to the leg and continuously bends and straightens the joint. This continuous motion is thought to reduce stiffness, ease pain, and keep extra scar tissue from forming inside the joint. The CPM is often used with a form of cold treatment that circulates cold water through hoses and pads around your knee.
Most ACL surgeries are now done on an outpatient basis. Many patients go home the same day as the surgery. Some patients stay one to two nights in the hospital if necessary. The tube placed in your knee at the end of the surgery is usually removed after 24 hours.
Your surgeon may also have you wear a protective knee brace for a few weeks after surgery. You'll use crutches for two to four weeks in order to keep your knee safe, but you'll probably be allowed to put a comfortable amount of weight down while you're up and walking.
Our Rehabilitation
What will my recovery be like?
Patients usually take part in formal physiotherapy after ACL reconstruction. When you begin your Kitchener Physiotherapy & Wellness program, the first few physiotherapy treatments are designed to help control the pain and swelling from the surgery. Our goal is to help you regain full knee extension as soon as possible.
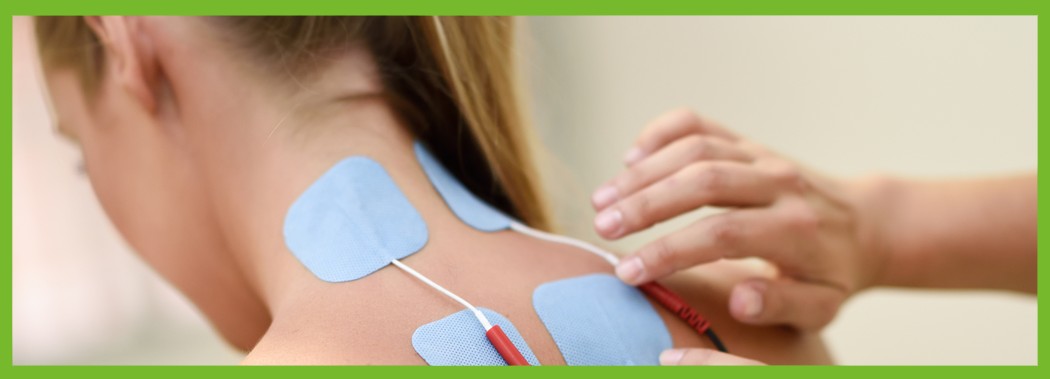
Following surgery, you may be told by your surgeon to avoid putting weight on the leg and limiting any active quadriceps contractions for up to six weeks. You may also have to wear a rigid brace at all times except when showering or during rehabilitatin for the first few weeks. Our physiotherapist will choose treatments to get the quadriceps muscles toned and active again when there is no risk to the graft or remaining patella tendon. Muscle stimulation and biofeedback, which involve placing electrodes over the quadriceps muscle, may be needed at first to get the muscle going again and to help retrain it.
As your Kitchener Physiotherapy & Wellness rehabilitation program evolves, we will choose more challenging exercises to safely advance your knee's strength and function. Our physiotherapist will use specialized balance exercises to help the muscles respond quickly and without thinking. This part of treatment is called neuromuscular training. If you need to stop suddenly, your muscles must react with just the right amount of speed, control, and direction. After ACL surgery, this ability doesn't come back completely without exercise.
Our neuromuscular training includes exercises to improve balance, joint control, muscle strength and power, and agility. Agility makes it possible to change directions quickly, go faster or slower, and improve starting and stopping. These are important skills for walking, running, and jumping, and especially for sports performance.
When you get full knee movement, your knee isn't swelling, and your strength and muscle control are improving, you'll be able to gradually go back to your work and sport activities. Our physiotherapists may recommend a functional brace for athletes who intend to return quickly to their sports.
Ideally, you'll be able to resume your previous lifestyle activities. However, athletes are usually advised to wait at least six months before returning to their sports. Most patients are encouraged to modify their activity choices.
Although the time required for recovery varies, you will probably be involved in a Kitchener Physiotherapy & Wellness progressive rehabilitation program for four to six months after surgery to ensure the best result from your ACL reconstruction. In the first six weeks following surgery, expect to see our physiotherapist two to three times a week. If your surgery and rehabilitation go as planned, you may only need to do a home program and see our physiotherapist every few weeks over the four to six month period.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Portions of this document copyright MMG, LLC.








 What does the surgeon hope to accomplish?
What does the surgeon hope to accomplish?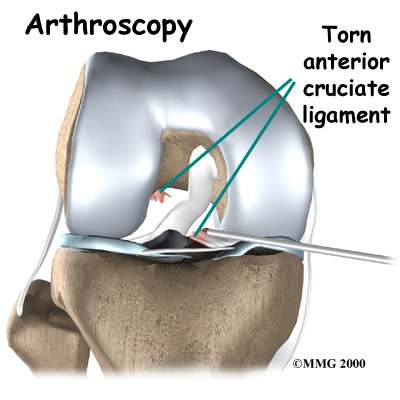 Most surgeons perform this surgery using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during
Most surgeons perform this surgery using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during