Introduction
Physiotherapy in Kitchener for Pain Care
Welcome to Kitchener Physiotherapy & Wellness guide to spinal cord stimulators.
 A spinal cord stimulator, also called a dorsal column stimulator, is an implanted electronic device used to help treat chronic pain. These devices have been in use for the treatment of pain for over 30 years and they continue to improve. The area of medical science responsible for developing these devices is called neuromodulation.
A spinal cord stimulator, also called a dorsal column stimulator, is an implanted electronic device used to help treat chronic pain. These devices have been in use for the treatment of pain for over 30 years and they continue to improve. The area of medical science responsible for developing these devices is called neuromodulation.
The spinal cord stimulator will not cure your pain, but you should see a reduction in your pain of 50 percent or more if the stimulator procedure is successful. The goal of the spinal cord stimulator is to allow you to be more active, have less pain, and take less pain medication.
This guide will help you understand:
- what parts of the spine are involved
- what the surgeon is trying to achieve
- what the spinal cord stimulator looks like
- what happens during surgery
- what could go wrong
- what Kitchener Physiotherapy & Wellness approach to rehabilitation is
Anatomy
What parts of the spine are involved?
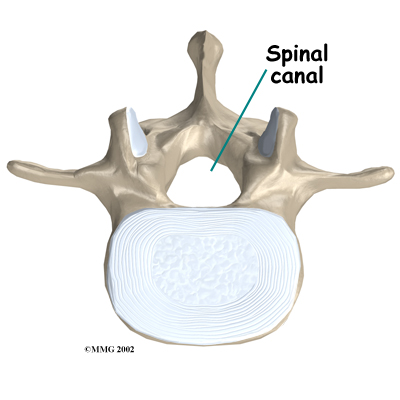
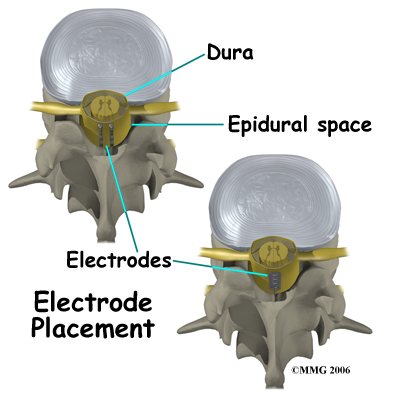
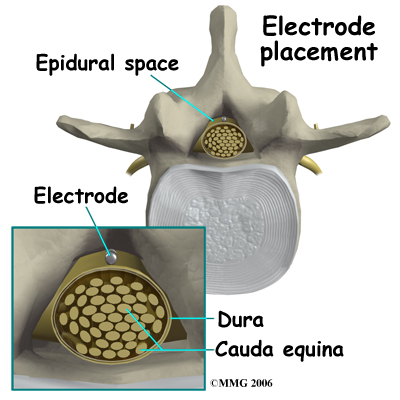
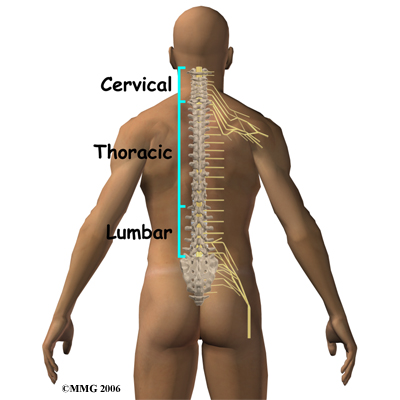
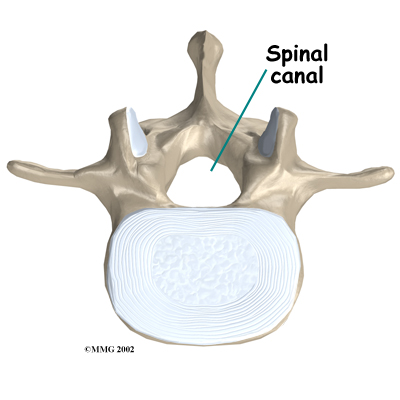
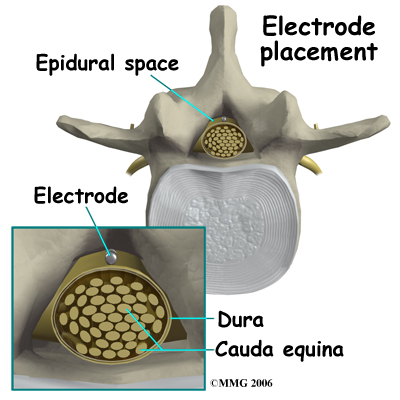
The spine is made up of 24 bones called vertebrae that stack on top of one another. Each vertebra is comprised of a ring of bone that encases and protects the spinal cord. When the vertebrae are stacked one on top of the other, these rings of bone create a hollow tube called the spinal canal. The spinal cord is a tube of nerve cells that create the motor and sensory pathways that link the brain to the body. The spinal cord runs through the spinal canal from the brain to the lower spine. Inside the spinal canal, a watertight sac called the dura covers the spinal cord. Inside the dura, the spinal cord is bathed by cerebral spinal fluid that cushions and protects the fragile nerve tissue.
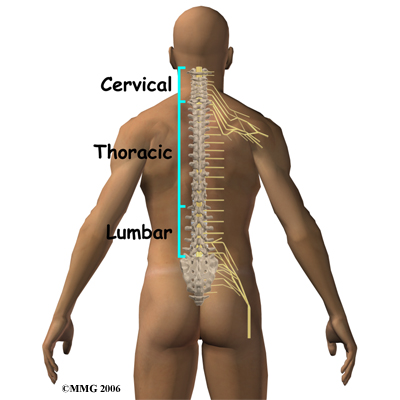
In between the vertebrae are intervertebral discs. The intervertebral discs cushion the spine and allow it to be flexible. The nerve roots exit the spinal canal between the vertebrae. The openings in the spinal canal where the nerve roots exit are called neuroforamen. If there is not enough room for the nerve roots to easily travel through these neuroforamen, this can lead to irritation and pressure on the nerves. This may cause symptoms of nerve dysfunction such as burning, pins and needles, and hypersensitivity. Pain from an irritated or pinched nerve root follows a pattern that matches where the nerve travels through the body. In the case of the lower or lumbar spine, these nerves travel into the lower extremities. In the neck these nerves travel into the arms and hands.
Rationale
What does my surgeon hope to achieve?
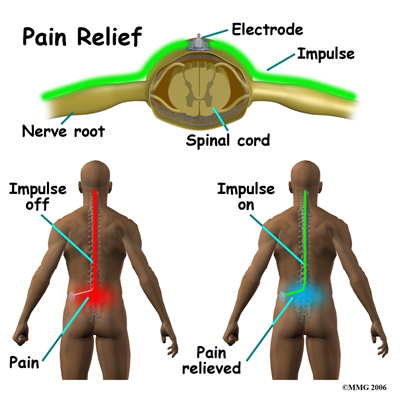
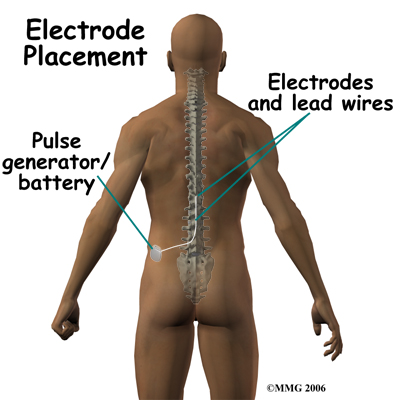
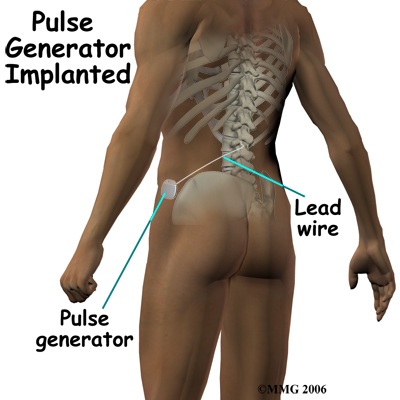
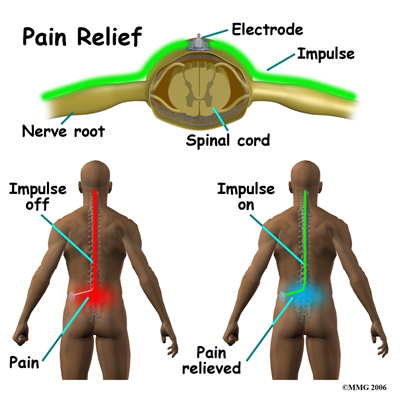
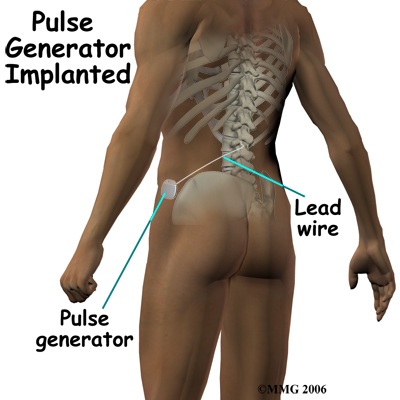
Spinal cord stimulation can be thought of as blocking the pain signal as it travels up the spinal cord to the brain. The small stimulator device is similar to a pacemaker and is implanted underneath the skin, usually in the lower abdomen or upper buttock. The device is connected to special electrodes that are positioned over the back of your spinal cord by wires placed inside the spinal canal. The stimulator device delivers an electrical current to the electrodes that interrupts the conduction of the pain signal, replacing the pain with a tingling, or buzzing sensation, which is often soothing. The electrical stimulation serves as a distraction and allows your brain to focus on the tingling rather than the painful pain signals.
 Spinal cord stimulation is usually considered as a treatment option when pain is chronic and severe, and injections, physiotherapy, medications, surgery, and other treatments have failed to give enough pain relief. The spinal cord stimulator will not cure your pain but you should expect a 50 percent or greater decrease in your pain following successful spinal cord stimulation. This should allow you to be more active, have less pain and require less pain medications.
Spinal cord stimulation is usually considered as a treatment option when pain is chronic and severe, and injections, physiotherapy, medications, surgery, and other treatments have failed to give enough pain relief. The spinal cord stimulator will not cure your pain but you should expect a 50 percent or greater decrease in your pain following successful spinal cord stimulation. This should allow you to be more active, have less pain and require less pain medications.
Spinal cord stimulation seems to work best for neuropathic pain, which is pain caused by injury or disease to nerves. Neuropathic pain can have many sources, for example: amputation leading to phantom limb pain, diabetes causing peripheral neuropathy, shingles leading to post herpetic neuropathy and injuries leading to chronic regional pain syndrome (CRPS). When the spinal nerve roots have been damaged due to constant pressure or irritation, this is also considered neuropathic pain. Neuropathic pain is difficult to treat. Medications have not been very effective in relieving this type of pain. Spinal cord stimulation is one technique that pain specialists find helps to reduce the symptoms of neuropathic pain.
Spinal cord stimulation has also been used to treat ongoing pain into the legs following back surgery. This condition is sometimes called Failed Back Surgery Syndrome. Spinal cord stimulation seems to be less helpful for back pain that does not have accompanying pain going into the legs.
Preparation
How should I prepare for surgery?
Before having the device implanted, you will need to undergo both a physical examination and a psychological evaluation.
There are several conditions that would prevent you from being considered a candidate for spinal cord stimulation.
If you have a pacemaker or cardioverter defibrillator already implanted, the spinal cord stimulator could interfere with this device and cause life threatening problems.
If you have a disease that requires that you take blood thinners you may be at too great a risk for bleeding into the spinal canal from the stimulator electrodes.
If you have any type of active infection, this will increase the risk of infection around the spinal stimulator. If the infection is cured, this contraindication may be removed.
Finally, if you have an untreated substance addiction or significant psychological problems, you may not be considered an appropriate candidate for the spinal cord stimulator until these problems are under optimal control.
To prepare for the procedure your doctor may tell you to remain "NPO" for a certain amount of time before the procedure. This means that you should not eat or drink anything for the specified amount of time before your procedure. This means no water, no coffee, no tea or anything. Nothing at all should be ingested. You may receive special instructions to take your usual medications with a small amount of water. Check with your doctor if you are unsure of what to do.
You may be instructed to discontinue certain medications that affect the clotting of your blood several days before the operation. This reduces the risk of excessive bleeding during and after the operation. These medications may include the common Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) such as aspirin, ibuprofen, naproxen and many other medications that are commonly used to treat arthritis. If you are taking any type of blood thinning medication you should let your doctor know. Medications used to prevent strokes, such as Plavix, can also affect blood clotting. These medications usually need to be stopped seven days prior to the procedure.
Wear loose fitting clothing that is easy to take off and put on. You may wish to take a shower the morning of the procedure using a bactericidal soap to reduce chances of infection. Do not wear jewelry or any type of scented oils or lotions.
Surgical Procedure
What happens during the surgery?
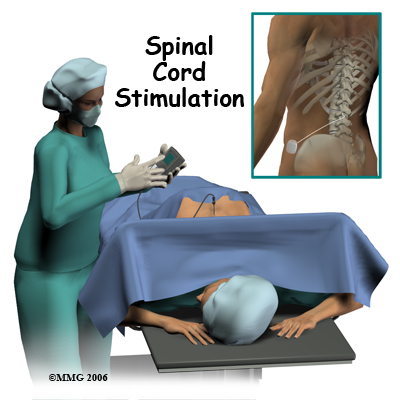
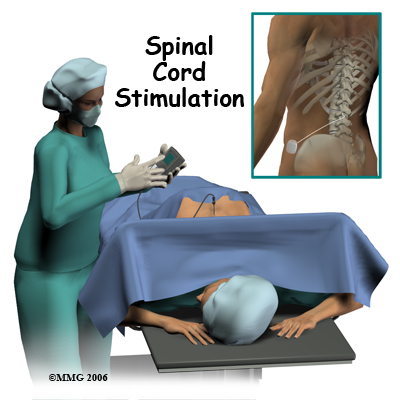
A surgeon, anesthesiologist, or other doctor who specializes in the treatment of pain does the implanting of the spinal cord stimulator.
 The complete spinal cord stimulation procedure is actually done in two stages. In the first stage, called the trial, the electrodes and wires are placed into position in the spinal canal and are left protruding through the skin. Think of this as similar to having an IV in your arm. The stimulator device can be connected to these wires and used to control the amount of spinal stimulation. The trial can last up to seven days while you test the amount of pain relief you get from using the device. If you and your doctor are pleased with the result and both of you consider the trial a success, you will be scheduled to have a second procedure where the device is implanted permanently under the skin. If you and your doctor are not pleased with the result and consider the trail a failure, the wires are removed and nothing remains inside your body. Being able to undergo a trial is one of the great benefits of spinal cord stimulation; you get to give the procedure a test drive before you commit to having the device permanently implanted.
The complete spinal cord stimulation procedure is actually done in two stages. In the first stage, called the trial, the electrodes and wires are placed into position in the spinal canal and are left protruding through the skin. Think of this as similar to having an IV in your arm. The stimulator device can be connected to these wires and used to control the amount of spinal stimulation. The trial can last up to seven days while you test the amount of pain relief you get from using the device. If you and your doctor are pleased with the result and both of you consider the trial a success, you will be scheduled to have a second procedure where the device is implanted permanently under the skin. If you and your doctor are not pleased with the result and consider the trail a failure, the wires are removed and nothing remains inside your body. Being able to undergo a trial is one of the great benefits of spinal cord stimulation; you get to give the procedure a test drive before you commit to having the device permanently implanted.
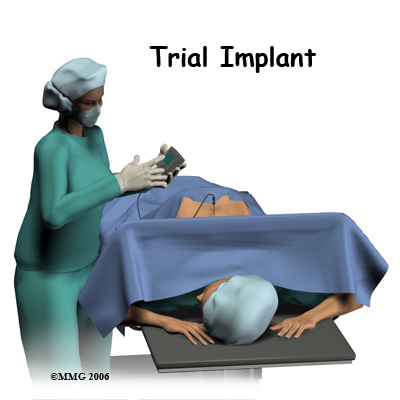 Both the trial implantation and the permanent implantation procedures usually take place in an operating room, either in a hospital or in a day surgery facility. An operating room is a sterile environment that decreases the risk of infection. Each procedure may last up to three hours. You should be able to go home the same day.
Both the trial implantation and the permanent implantation procedures usually take place in an operating room, either in a hospital or in a day surgery facility. An operating room is a sterile environment that decreases the risk of infection. Each procedure may last up to three hours. You should be able to go home the same day.
To perform the procedure, you will be given an intravenous sedative to help you relax and a local anesthetic will be used to numb the area where the wires are inserted. A general anesthetic is not normally used, especially during the procedure for the trial implantation. You will need to be awake so that you can help guide your doctor when adjusting the device in order to provide the best pain relief.
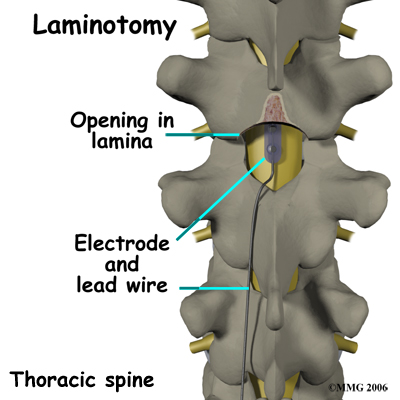
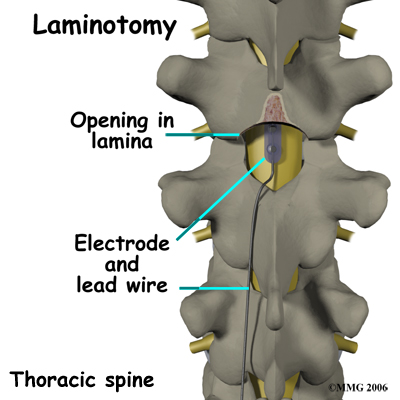
Placement of temporary wires for the trial is a minimally invasive procedure. An epidural needle is placed through the skin and into the spinal canal near the spinal cord. This is done with the help of a special X-ray called fluoroscopy. The electrode wires are then inserted through a needle and pushed through the spinal canal until they are in the right position. The wires are then attached to the external stimulator device. Your surgeon will adjust the wires and tune the stimulator. When satisfied with the placement of the wires, a stitch to your skin is used to keep the electrode wires in place for the trial period. You are able to adjust the strength of the electrical stimulation and turn it off and on using the external device. When the stimulator is on, you should feel a tingling sensation that covers the area of your pain.
If the trial is successful, you will undergo a second procedure that involves placement of the electrode wires near the spinal cord.
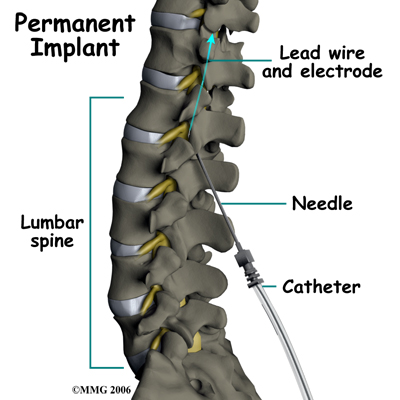
The procedure for permanent placement of the spinal stimulator is very similar to the trial. The new electrodes can be placed in the same way using the needle technique, or if more precise placement is needed a small incision may be necessary over the spine. The wires are then tunneled under the skin to the area where a small incision is made to place the stimulator device under the skin. If your pain is in your legs, an incision for the device is made on your lower abdomen or upper buttock and the wires are placed in the low back.
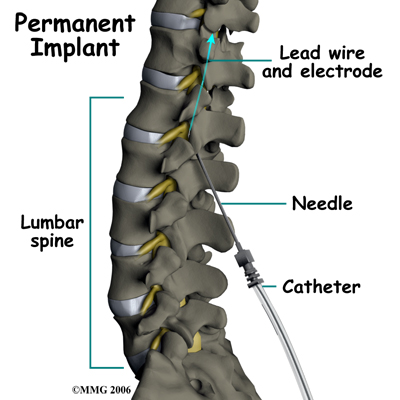
 For pain involving the arms, an incision for the device is made on the side of the chest and the wires are placed in the upper back.
For pain involving the arms, an incision for the device is made on the side of the chest and the wires are placed in the upper back.
A wireless controller that you should keep with you at all times controls the stimulator device. The controller allows the stimulator to be programmed to adjust the type and strength of the electric stimulation. The spinal cord stimulator is not necessarily permanent and may be removed if necessary. The battery generally lasts two to five years at which time the device must be removed surgically and the battery or the device replaced.
After Care
What happens after the procedure?
You will need to lie down as much as possible for 12 hours following your surgery. Your surgeon will allow you to take pain medication for the first few days following surgery. Narcotic pain medications can cause constipation and laxatives may be necessary to have regular bowel movements. You may be asked to avoid the use of an anti-inflammatory such as aspirin, ibuprofen, or naproxen, as they can cause bleeding.
You will be asked to avoid bending, twisting, stretching, reaching overhead, or lifting objects over five pounds for the first six to eight weeks. This is to avoid movement of the wires that connect the device to the electrodes. You will probably not be allowed to drive for two to four weeks after the procedure. Sexual activity may also be restricted initially.
You should expect some mild swelling and bruising at the incision site. Ice packs may help with pain and swelling. There will be sutures or staples and a dressing covering the incision. Call your doctor immediately if you run a temperature, or notice redness, swelling, separation, or drainage from the incision, which can all indicate that an infection has developed.
You will be allowed to shower but you should not bathe or submerge your incisions for four weeks. Watch for visible swelling or leaking of fluid from the incisions. You should wear loose clothing over the incision sites. If you should have sudden weakness of your legs, loss of bowel or bladder function, or sudden severe back pain, you should call your surgeon and go to the emergency department. It may indicate pressure on the spinal cord, a complication that could require emergency surgery.
You will be given instructions on how to operate your spinal cord stimulator. Usually one or two hours of stimulation, three to four times a day is enough to relieve pain for the rest of the day. You should expect 50 to 70 percent improvement in your pain. The device should be turned off when driving and operating machinery or power tools. Electronic systems that contain magnets will need to be avoided as they can interfere with the electrical current from your device. These include security systems found in libraries and airports. Strong X-rays, ultrasound, and magnetic resonance imaging (MRI) should also be avoided. Microwaves, cell phones, pagers, and anti-theft sensors will not affect your stimulator. You will be given an identification card that can be shown to airport and other security officials when necessary. The ID card can also be used in the event of a medical emergency, as it is important for medical providers to know about the implanted device.
You will have a follow up appointment with your doctor seven to 10 days after surgery to remove sutures or staples. Your surgeon may make adjustments to the device at this and other follow-up appointments.
Rehabilitation
Physiotherapy at Kitchener Physiotherapy & Wellness after spinal cord stimulation implantation surgery can begin as soon as your surgeon recommends it. Learning to activate the deep muscles of the abdomen and low back area (core) that support the spine can be done nearly immediately without putting stress on the implanted stimulator or electrodes; no twisting, bending, or stretching is required. Your therapist will teach you how to activate these muscles with an isometric contraction where you tighten the muscles but don’t move the trunk. They will ask you to gently contract these muscles as you do your daily activities. These core muscles, when activated, work like an internal brace that help to support the spine. You may have learned how to use these muscles during physiotherapy treatment prior to the spinal cord stimulator being implanted. After the implantation, activating these muscles may feel different due to a decreased level of pain. You will likely be able to more effectively activate these muscles due to the lower level of pain you feel, which will be beneficial for you back problem overall. For this reason, it is important to follow up with your physiotherapist after the surgical implantation despite any therapy you have undertaken prior to the surgery. In addition, the surgical incision and procedure itself is considered a new ‘controlled injury’, which in itself affects the ability to activate and control your trunk muscles so re-learning to use these muscles post-implantation is essential. Physiotherapy at Kitchener Physiotherapy & Wellness can ensure that you are using the muscles as effectively as possible to support the spine after your implantation surgery.
Further physiotherapy treatment will usually not be commenced until after the 6-8 week mark when your restrictions as outlined above have been lifted. This amount of time allows scar tissue to form around the electrodes and wires in order to keep them in place before doing any significant movements with your trunk and back. Your surgeon will advise you when the appropriate time to lift the restrictions in your individual case is.
Once it is safe to do so your physiotherapist will assess other important areas of your body that help to support the spine, such as your hips. They will assess both the range of motion of your hips as well as the ability of your gluteal (buttocks) muscles to support the hips and back. If your hip range of motion is poor or your gluteals are not strong enough then extra stress is transferred to your low back. Often because you feel less pain in your back after having the spinal cord stimulator implanted you can more effectively strengthen your buttocks muscles than previous to the implantation. The flexibility of the anterior hip muscles as well as the muscles of the front and back of your thigh will also be assessed and stretches may be provided if any muscles are found to be tight or overactive.
Your physiotherapist will also assess your posture and overall alignment, which again is important to address once your pain is at a more controlled level. Many bad posturing habits can develop simply due to chronic pain. With your pain more under control, addressing these habits and establishing new and more efficient postural positions and ways of moving is essential. Overall alignment of your trunk and lower extremities will be reviewed and, if necessary, any issues in your knees or ankles contributing to poor alignment (which can affect your back) will be addressed.
In addition to your posture your gait will also be reviewed. Pain does not only affect your static posture but can also cause you to develop an inefficient walking pattern that puts unnecessary stress on joints in the lower extremities and the back. In a normal day most people take thousands of steps just to get around therefore an inefficient or improper walking pattern can quickly lead to pain either in the back itself or other related joints. Your physiotherapist will assess your gait and ensure that you are walking properly.
After approximately six to eight weeks, you will be able increase your activity level and start to resume more of your normal activities. Your physiotherapist will advance your core strengthening exercises at this time frame so that you are doing challenging exercises that progress your strength and endurance without putting any stress on your back. They will also advise you on returning to your regular daily work and leisure activities. As soon as it is safe to, they will encourage you to partake in some cardiovascular activity to maintain your overall fitness. Often stationary cycling where you sit upright rather than bending over is manageable as an exercise early on after implantation, as is walking. Cardiovascular exercises in the pool may also be suggested but should not be done until the incision wound has healed and your surgeon has given you clearance to do so. The hydrostatic properties of water as well as the warmth of a physiotherapy pool often make exercise less painful so they are encouraged. It should be noted though, that some spinal stimulators should not be used on stimulation mode while in the pool. Your surgeon can advise you regarding your particular brand of stimulator and its specific activity restrictions.
Participating in more stressful cardiovascular activities such as jogging, weight lifting, or regular sport will need to be discussed with your surgeon to ensure that it is safe to do so in your case. Any jolts of pain or inconsistent sensations may mean your electrodes or wires are shifting slightly; this issue will need to be reviewed by your surgeon.
You will be required to do your rehabilitation exercises as part of a home exercise program. As you become more independent with the exercises and once your therapist is confident that you are progressing as they would expect you to, your visits to Kitchener Physiotherapy & Wellness will become less frequent, and your therapist will act only as a guide.
Should your pain flare up during certain intervals, you may need to follow up with your physiotherapist more frequently until the pain settles.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Complications
What might go wrong?
Spinal cord stimulation is considered minimally invasive and safe, however there are several complications that may occur during or after this procedure. No invasive procedure is 100 percent foolproof. Complications are uncommon, but you should know what to watch for it they occur.
Infection can occur at the incision site, around the wires, or around the device itself. You should watch for signs of increasing redness, swelling, pain and fever. Almost all infections will need to be treated with antibiotics. When the infection involves the spinal canal, it may be more serious. A condition called an epidural abscess may form inside the spinal canal. This infection can cause a large pocket of pus to form around the nerves putting too much pressure on the nerves. If this complication occurs, you will probably need a surgical procedure to drain the infection and remove the pressure from the nerves. The device, the electrodes and the wires will need to be removed. Antibiotics will also be necessary to treat the infection.
An epidural hematoma can occur which happens due to excessive bleeding into the spinal canal. The bleeding can cause pressure on the spinal cord. This, in turn, can cause paralysis or loss of movement of the limbs. Loss of bowel and bladder function can also occur. This complication requires emergency surgery to drain the hematoma and relieve the pressure. The spinal cord damage can be permanent.
A pneumothorax is the collapse of a lung. A lung can be punctured when needles are inserted in the area of the chest or upper back. If the pneumothorax is small, then it may only require monitoring for several days until it resolves. If it is severe and interferes with your breathing, a chest tube may need to be inserted to re-inflate the lung.
Damage to the spinal sac during the insertion of the electrodes may cause a persistent spinal fluid leak. The symptom that you will experience if this occurs is a very bad headache. The headache is worse when you are sitting or standing upright. It may cause nausea and vomiting and will go away if you lie flat or with your head a bit lower that your feet. The headache occurs because the spinal fluid pressure in the skull decreases. This is the reason why the headache goes away when you lie down; the spinal fluid pressure goes back to normal in your skull. Most spinal headaches go away in a few days when the hole in the spinal sac heals and closes on its own. You may be instructed to stay flat for a couple of days until this occurs. If your headache lasts longer than 48 hours despite lying down as instructed, call your surgeon. In some cases a spinal fluid leak may require surgery to correct.
Nerve damage caused by needles and electrodes placed in the area of the spinal cord may occur. Even paralysis that could be permanent can occur.
Allergic reactions can occur, usually to medications or dye used during the surgery. A severe allergic reaction called anaphylaxic shock can be deadly.
A seroma is the collection of fluid that develops in the pocket around the implanted device. It can last several weeks or months. Your surgeon can drain the fluid. If the fluid in the seroma becomes infected, the device must be removed and the infected fluid drained.
Finally, technical problems or failure of the device can occur. The electrodes may slip out of position. This may change the area of stimulation and could reduce or eliminate the effectiveness of the pain relief. The wires or the electrodes can break leading to failure of the device.
It is important to remember that the spinal cord stimulator is not a cure for your pain; it is only a part of your overall pain management plan. Along with using the device you will still need to continue working with the other recommendations from your therapist, surgeon, and other healthcare professionals in your pain management team.
Portions of this document copyright MMG, LLC.
 A spinal cord stimulator, also called a dorsal column stimulator, is an implanted electronic device used to help treat chronic pain. These devices have been in use for the treatment of pain for over 30 years and they continue to improve. The area of medical science responsible for developing these devices is called neuromodulation.
A spinal cord stimulator, also called a dorsal column stimulator, is an implanted electronic device used to help treat chronic pain. These devices have been in use for the treatment of pain for over 30 years and they continue to improve. The area of medical science responsible for developing these devices is called neuromodulation.








 Spinal cord stimulation is usually considered as a treatment option when pain is chronic and severe, and injections, physiotherapy, medications, surgery, and other treatments have failed to give enough pain relief. The spinal cord stimulator will not cure your pain but you should expect a 50 percent or greater decrease in your pain following successful spinal cord stimulation. This should allow you to be more active, have less pain and require less pain medications.
Spinal cord stimulation is usually considered as a treatment option when pain is chronic and severe, and injections, physiotherapy, medications, surgery, and other treatments have failed to give enough pain relief. The spinal cord stimulator will not cure your pain but you should expect a 50 percent or greater decrease in your pain following successful spinal cord stimulation. This should allow you to be more active, have less pain and require less pain medications. The complete spinal cord stimulation procedure is actually done in two stages. In the first stage, called the trial, the electrodes and wires are placed into position in the spinal canal and are left protruding through the skin. Think of this as similar to having an IV in your arm. The stimulator device can be connected to these wires and used to control the amount of spinal stimulation. The trial can last up to seven days while you test the amount of pain relief you get from using the device. If you and your doctor are pleased with the result and both of you consider the trial a success, you will be scheduled to have a second procedure where the device is implanted permanently under the skin. If you and your doctor are not pleased with the result and consider the trail a failure, the wires are removed and nothing remains inside your body. Being able to undergo a trial is one of the great benefits of spinal cord stimulation; you get to give the procedure a test drive before you commit to having the device permanently implanted.
The complete spinal cord stimulation procedure is actually done in two stages. In the first stage, called the trial, the electrodes and wires are placed into position in the spinal canal and are left protruding through the skin. Think of this as similar to having an IV in your arm. The stimulator device can be connected to these wires and used to control the amount of spinal stimulation. The trial can last up to seven days while you test the amount of pain relief you get from using the device. If you and your doctor are pleased with the result and both of you consider the trial a success, you will be scheduled to have a second procedure where the device is implanted permanently under the skin. If you and your doctor are not pleased with the result and consider the trail a failure, the wires are removed and nothing remains inside your body. Being able to undergo a trial is one of the great benefits of spinal cord stimulation; you get to give the procedure a test drive before you commit to having the device permanently implanted.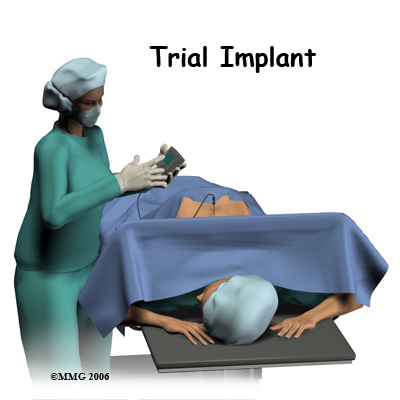 Both the trial implantation and the permanent implantation procedures usually take place in an operating room, either in a hospital or in a day surgery facility. An operating room is a sterile environment that decreases the risk of infection. Each procedure may last up to three hours. You should be able to go home the same day.
Both the trial implantation and the permanent implantation procedures usually take place in an operating room, either in a hospital or in a day surgery facility. An operating room is a sterile environment that decreases the risk of infection. Each procedure may last up to three hours. You should be able to go home the same day.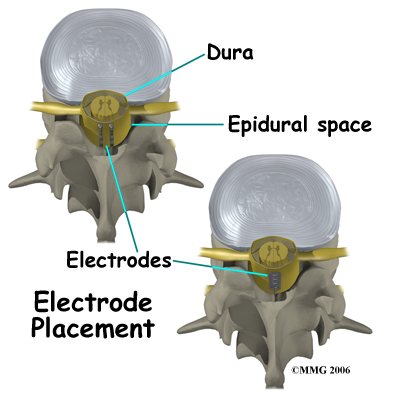
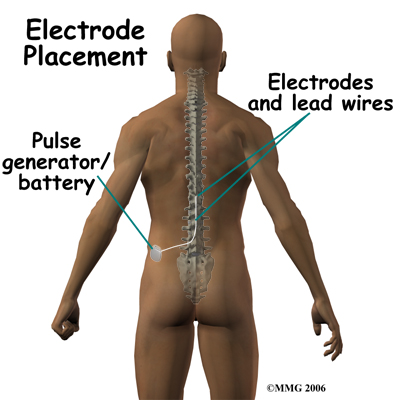
 For pain involving the arms, an incision for the device is made on the side of the chest and the wires are placed in the upper back.
For pain involving the arms, an incision for the device is made on the side of the chest and the wires are placed in the upper back.