Introduction
Physiotherapy in Kitchener for Lower Back
Welcome to Kitchener Physiotherapy & Wellness patient resource about Lumbar Spondylolisthesis.
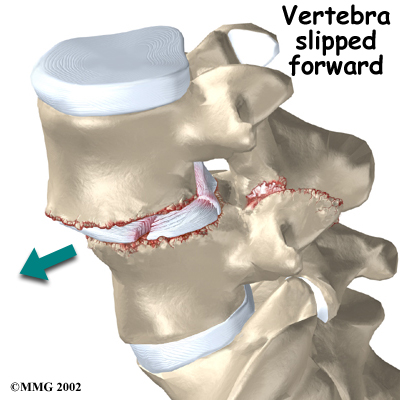
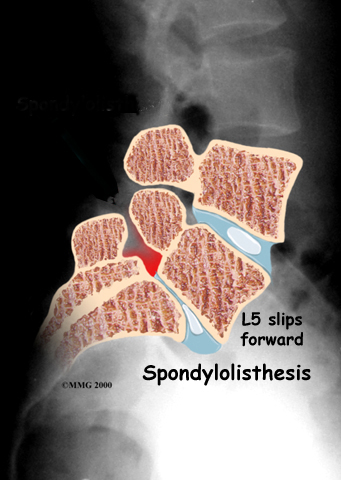
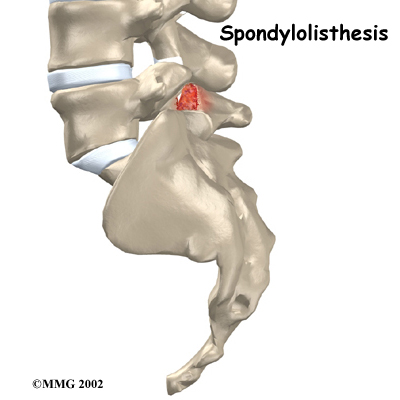
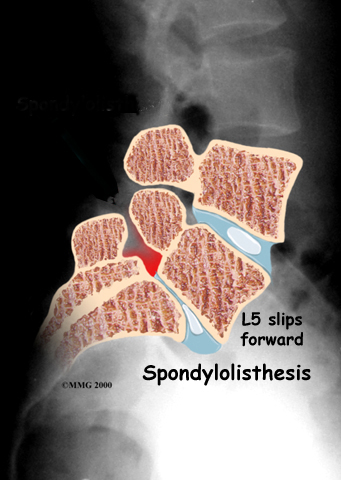
Normally, the bones of the spine (the vertebrae) stand neatly stacked on top of one another. Ligaments and joints support the spine. Spondylolisthesis alters the alignment of the spine. In this condition, one of the spine bones slips forward over the one below it. As the bone slips forward, the nearby tissues and nerves may become irritated and painful.
This article will help you understand:
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the spine are involved?
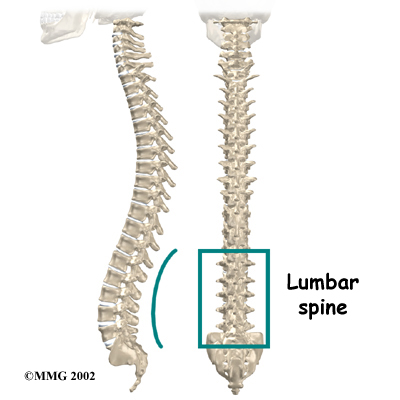
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to create the . The spinal column gives the body its form. It is the body's main upright support. The section of the spine in the lower back is called the lumbar spine.
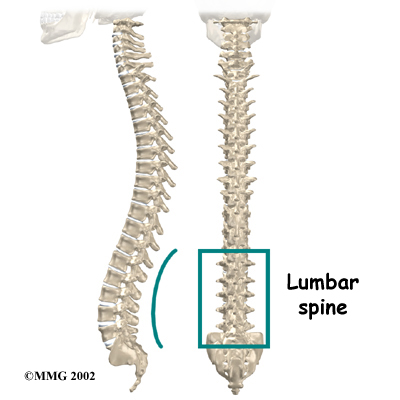
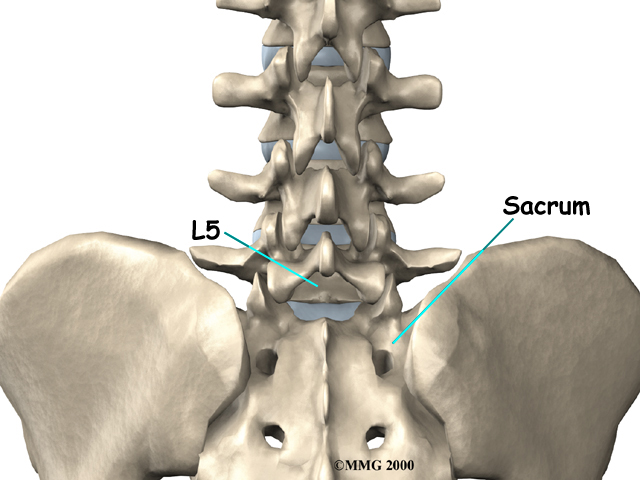
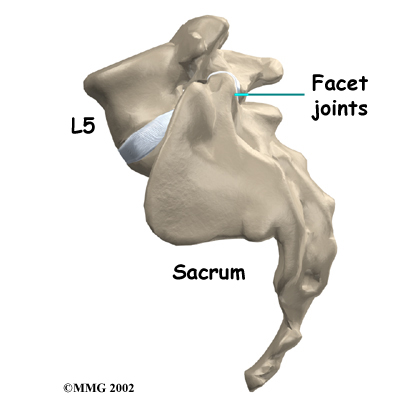
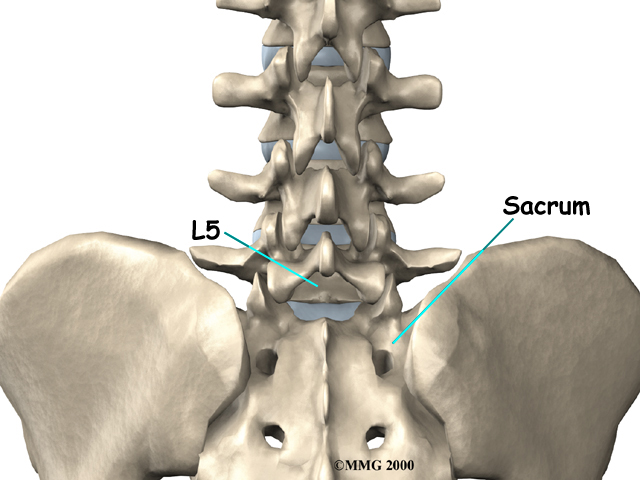
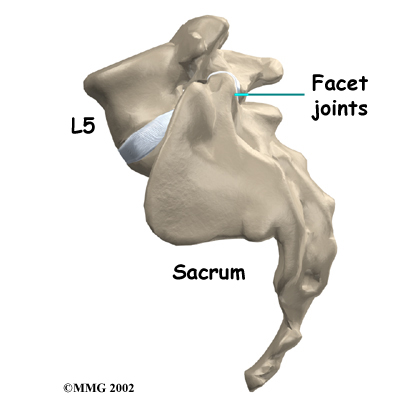
The lumbar spine is made of the lower five vertebrae. Doctors often refer to these vertebrae as L1 to L5. These five vertebrae line up to give the low back a slight inward curve. The of the lumbar spine, L5, connects to the top of the sacrum, a triangular bone at the base of the spine that fits between the two pelvic bones.
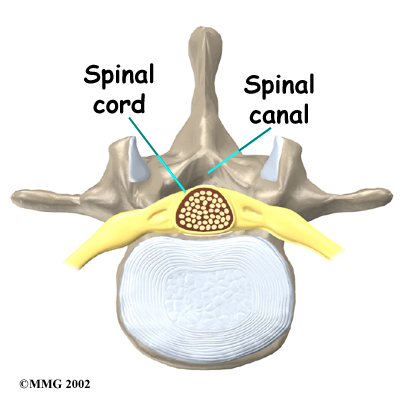
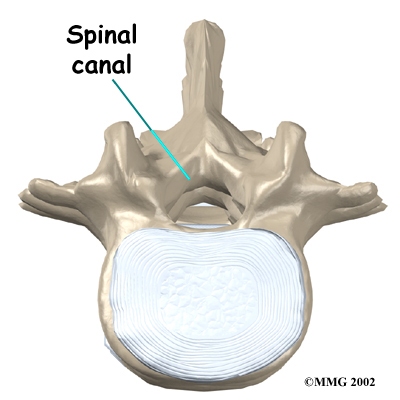
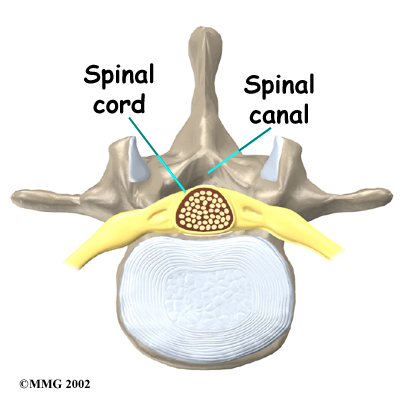
Each vertebra is formed by a round block of bone, called a vertebral body. A attaches to the back of the vertebral body. When the vertebrae are stacked on top of each other, these bony rings create a hollow tube. This tube, called the spinal canal, surrounds the as it passes through the spine. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
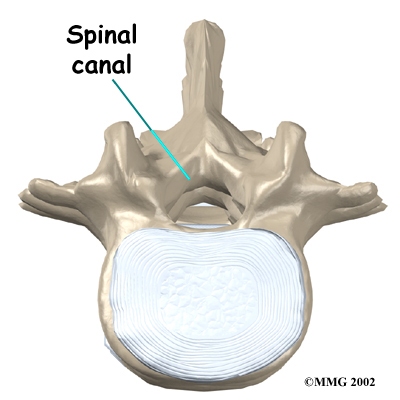
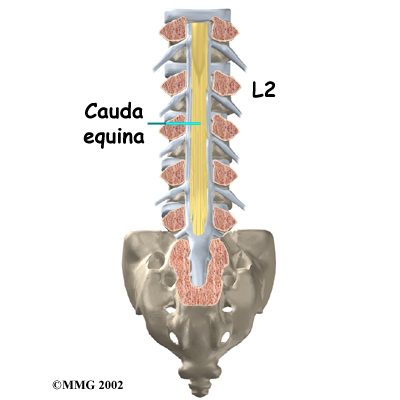
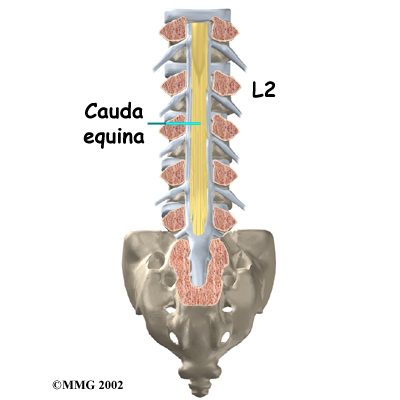
The spinal cord only extends to L2. Below this level, the spinal canal encloses a bundle of nerves that goes to the lower limbs and pelvic organs. The Latin term for this bundle of nerves is , meaning horse's tail.
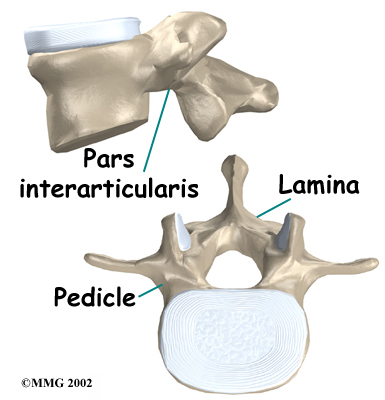
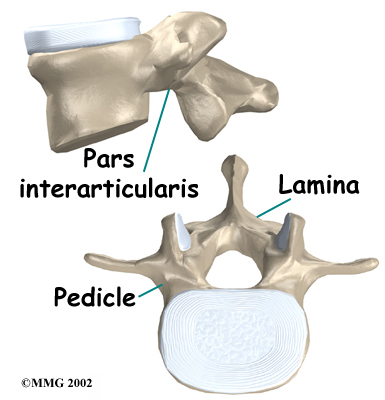
Two sets of bones form the spinal canal's . Two pedicle bones attach to the back of each vertebral body. Two lamina bones complete the ring. The place where the lamina and pedicle bones meet is called the pars interarticularis, or pars for short. There are two such meeting points on the back of each vertebra, one on the left and one on the right. The pars is thought to be the weakest part of the bony ring.
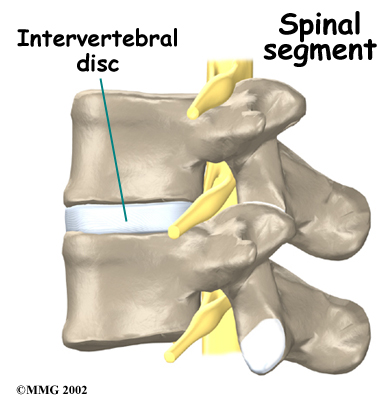
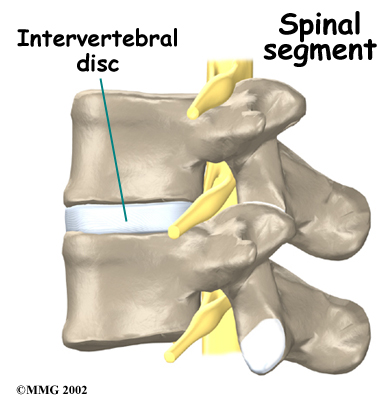
Intervertebral discs separate the vertebral bodies. The discs normally work like shock absorbers. They protect the spine against the daily pull of gravity. They also protect the spine during strenuous activities that put strong force on the spine, such as jumping, running, and lifting.
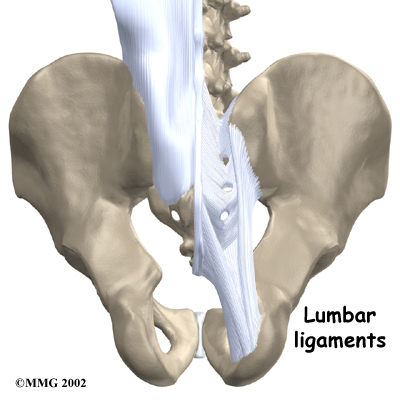
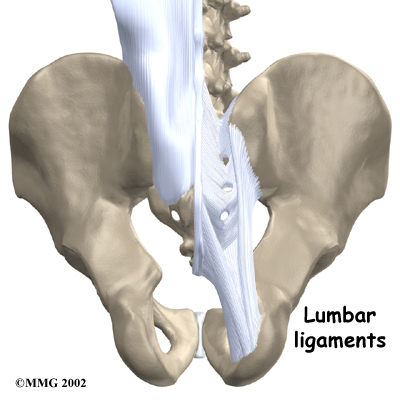
The lumbar spine is supported by ligaments and muscles. The ligaments, which connect bones together, are arranged in layers and run in multiple directions. connect the bones of the lumbar spine to the sacrum (the bone below L5) and pelvis.
Between the vertebrae of each spinal segment are two . The facet joints are located on the back of the spinal column. There are two facet joints between each pair of vertebrae, one on each side of the spine. A facet joint is made of small, bony knobs that line up along the back of the spine. Where these knobs meet, they form a joint that connects the two vertebrae. The alignment of the facet joints of the lumbar spine allows freedom of movement as you bend forward and back.
The anatomy of the lumbar spine is often discussed in terms of . Each spinal segment includes two vertebrae separated by an intervertebral disc, the nerves that leave the spinal cord at that level, and the facet joints that link each level of the spinal column.
Related Document: Kitchener Physiotherapy & Wellness Guide to Lumbar Spine Anatomy
Causes
Why do I have this problem?
Spondylolisthesis may very rarely be congenital, which means it is present at birth. It can also occur in childhood as a result of injury. In older adults, degeneration of the disc and facet (spinal) joints can lead to spondylolisthesis.
Spondylolisthesis from degeneration usually affects people over 50 years old. This condition occurs in African Americans more often than in whites. Women are affected more often than men. The effect of the female hormone estrogen on ligaments and joints is to cause laxity or looseness. The higher levels of estrogen in women may account for the greater incidence of spondylolisthesis. Degenerative spondylolisthesis mainly involves slippage of L4 over L5.
In younger patients (under 20 years old), spondylolisthesis usually involves slippage of the fifth lumbar vertebra over the top of the sacrum. There are several reasons for this. First, the connection of L5 and the sacrum forms an angle that is tilted slightly forward, mainly because the top of the sacrum slopes forward. Second, the slight inward curve of the lumbar spine creates an additional forward tilt where L5 meets the sacrum. Finally, gravity attempts to pull L5 in a forward direction.
 Facet joints are small joints that connect the back of the spine together. Normally, the facet joints connecting L5 to the sacrum create a solid buttress to prevent L5 from slipping over the top of the sacrum. However, when problems exist in the disc, facet joints, or bony ring of L5, the buttress becomes ineffective. As a result, the L5 vertebra can slip forward over the top of the sacrum.
Facet joints are small joints that connect the back of the spine together. Normally, the facet joints connecting L5 to the sacrum create a solid buttress to prevent L5 from slipping over the top of the sacrum. However, when problems exist in the disc, facet joints, or bony ring of L5, the buttress becomes ineffective. As a result, the L5 vertebra can slip forward over the top of the sacrum.
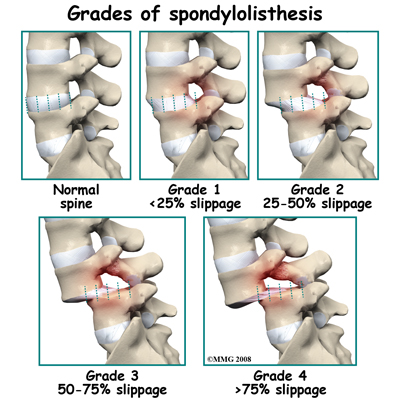
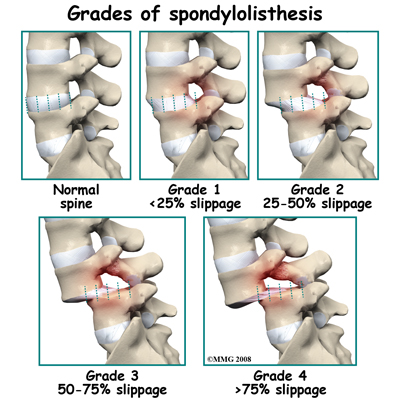
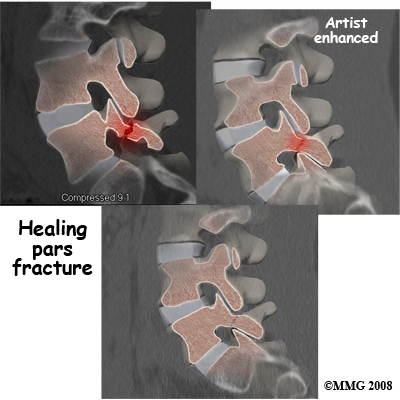
A condition called spondylolysis can lead to the slippage that happens with spondylolisthesis. Spondylolysis is a defect in the bony ring of the spinal column. It affects the pars interarticularis, mentioned earlier. This defect is most commonly thought to be a stress fracture that happens from repeated strains on the bony ring. Participants in gymnastics and football commonly suffer these strains. Spondylolysis can lead to the spine slippage when a fracture occurs on both sides of the bony ring. This slippage is called spondylolisthesis. The slippage is from I through IV, one being mild, IV often causing neurological symptoms. The back section of the bony ring separates from the main vertebral body, so the injured vertebra is no longer connected by bone to the one below it. In this situation, the facet joints can't provide their normal support. The vertebra on top is then free to slip forward over the one below.
Related Document: Kitchener Physiotherapy & Wellness Guide to Spondylolysis
A traumatic fracture in the bony ring can lead to slippage when the fracture goes completely through both sides of the bony ring. The facet joints are no longer able to provide a buttress, allowing the vertebra with the crack in it to slip forward. This is similar to what happens when spondylolysis (mentioned earlier) occurs on both sides of the bony ring, but in this case it happens all at once.
Degenerative changes in the spine (those from wear and tear) can also lead to spondylolisthesis. The spine ages and wears over time, much like hair turns gray. These changes affect the structures that normally support healthy spine alignment. Degeneration in the disc and facet joints of a spinal segment causes the vertebrae to move more than they should. The segment becomes loose, and the added movement takes an additional toll on the structures of the spine. The disc weakens, pressing the facet joints together. Eventually, the support from the facet joints becomes ineffective, and the top vertebra slides forward.
Symptoms
What does the condition feel like?
An ache in the low back and buttock areas is the most common complaint in patients with spondylolisthesis. Pain is usually worse when standing, walking, or bending backward and may be eased by resting or bending the spine forward. Leaning on a counter top, piece of furniture, or shopping cart are common ways to alleviate (reduce) the symptoms.
Spasm is also common in the low back muscles. The hamstring muscles on the back of the thighs may become tight.
 The pain can be from mechanical causes. Mechanical pain is caused by wear and tear on the parts of the spine. When the vertebra slips forward, it puts a painful strain on the disc and facet joints.
The pain can be from mechanical causes. Mechanical pain is caused by wear and tear on the parts of the spine. When the vertebra slips forward, it puts a painful strain on the disc and facet joints.
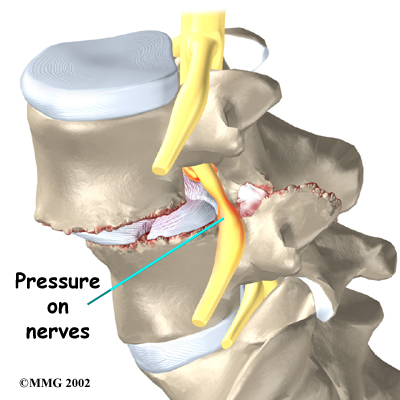
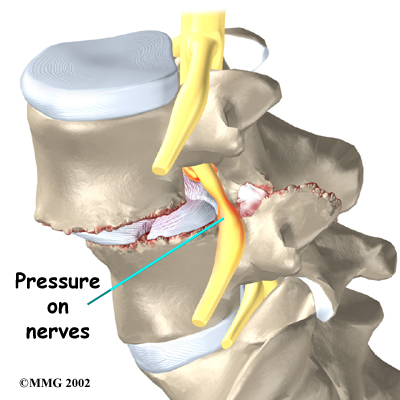
Slippage can also cause nerve compression. Nerve compression is a result of . As the spine slips forward, the nerves may be squeezed where they exit the spine. This condition also reduces space in the spinal canal where the vertebra has slipped. This can put extra pressure on the nerve tissues inside the canal. Nerve compression can cause symptoms where the nerve travels and may include numbness, tingling, slowed reflexes, and muscle weakness in the legs.
Nerve pressure on the cauda equina (mentioned earlier), the bundle of nerve roots within the lumbar spinal canal, can affect the nerves that go to the bladder and rectum. When this happens, bowel and/or bladder function can be affected. The pressure may cause low back pain, pain running down the back of both legs, and numbness or tingling between the legs in the area you would contact if you were seated on a saddle.
Diagnosis
How do health care providers diagnose the problem?
Diagnosis begins with a complete history and physical exam. When you first visit Kitchener Physiotherapy & Wellness, we will ask questions about your symptoms and how your problem is affecting your daily activities. Our physiotherapist will also want to know what positions or activities make your symptoms worse or better.
Next, our physiotherapist will examine you by checking your posture and the amount of movement in your low back. We check to see which back movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are also tested.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physiotherapists at Kitchener Physiotherapy & Wellness have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Our Treatment
Non-surgical Rehabilitation
Back pain associated with spondylolisthesis will gradually improve in up to one-third of all patients. Slippage of one vertebra over the other does not increase in this group, and worsening of symptoms is not expected in patients who don’t have neurologic symptoms at the time of diagnosis.
Nonsurgical treatment for spondylolisthesis commonly involves physiotherapy, such as that offered at Kitchener Physiotherapy & Wellness. Although the time required for recovery is different for each patient, our physiotherapist may recommend that you attend physiotherapy session a few times each week for four to six weeks. In some cases, patients may need a few additional weeks of care.
Our physiotherapist may ask that you rest your back by limiting your activities. This is to help decrease inflammation and calm muscle spasm. You may need to take time away from sports or other strenuous activities to give your back a chance to heal.
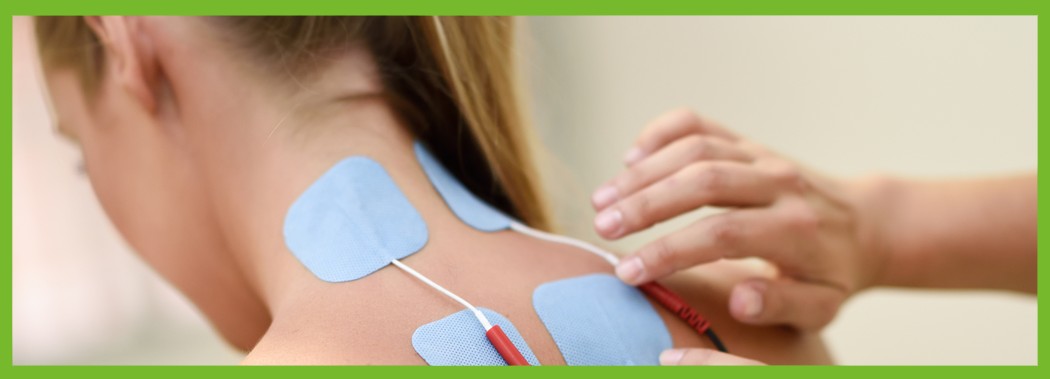
The first goal of treatment is to control symptoms. Our physiotherapist works with you to find positions and movements that ease pain. Treatments of heat, cold, ultrasound, and electrical stimulation may be used to calm pain and muscle spasm. We will show you how to stretch tight muscles, especially the hamstring muscles on the back of the thigh.
Your physiotherapist can assign positions and exercises to ease your symptoms. We can design a personalized exercise program to improve flexibility in your low back and hamstrings and to strengthen your back and abdominal muscles.
The use of a stationary bike can promote aerobic conditioning and puts you in the optimal position to open the spaces where the nerve roots exit. This type if exercise program can aid in reducing the painful symptoms.
If your doctor diagnoses an acute pars fracture that has the potential to heal, it may be recommended that you wear a rigid back brace for a few months. This usually occurs in children and teenagers who begin having back pain and see their doctor early on.
As you recover, our physiotherapist will gradually advance you in a series of strengthening exercises for the abdominal and low back muscles. Working these core muscles helps patients move easier and lessens the chances of future pain and problems.

A primary purpose of your physiotherapy is to help you learn how to take care of your symptoms and prevent future problems. You'll be given a home program of exercises to continue improving flexibility, posture, endurance, and low back and abdominal strength. Our physiotherapist will also describe strategies you can use if your symptoms flare up.
Post-surgical Rehabilitation
Rehabilitation after surgery is more complex. Patients who have surgery for spondylolisthesis usually stay in the hospital for a few days afterward.
Some surgeons require patients to wear a rigid brace or cast for up to four months after fusion surgery for spondylolisthesis. Patients who've had fusion surgery for a severe slip may also be required to stay off their feet for a period of time.
After lumbar fusion surgery for spondylolisthesis, patients must normally wait four months before beginning our rehabilitation program. This delay is needed to give the fusion a chance to start healing. Although time required for recovery is different for each patient, Kitchener Physiotherapy & Wellness patients typically need to attend physiotherapy sessions for six to eight weeks and should expect full recovery to take at least 12 months.
Ideally, our patients are eventually able to return to their previous activities. However, some patients may need to modify or discontinue certain activities to avoid future problems.
When your recovery is well under way, your regular visits to Kitchener Physiotherapy & Wellness will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Physician Review
With cases of lumbar spondylolisthesis, doctors will usually order of the low back. The X-rays are taken with your spine in various positions. They can be used to see which vertebra is slipping and how far it has slipped.
If more information is needed, your doctor may order computed tomography (a CT scan). This is a detailed X-ray that lets the doctor see slices of the body's tissue. If you have nerve problems, the doctor may combine the CT scan with myelography. To do this, a special dye is injected into the space around the spinal canal, the subarachnoid space. During the CT scan, the dye highlights the spinal nerves. The dye can improve the accuracy of a standard CT scan for diagnosing the health of the nerves.
Your doctor may also order a magnetic resonance imaging (MRI) scan. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. It can help in the diagnosis of spondylolisthesis. It can also provide information about the health of nerves and other soft tissues.
Studies have not been done yet to determine the best treatment for this condition. Conservative care is preferred, especially when the vertebra hasn't slipped very far. Most patients with symptoms from degenerative spondylolisthesis do not need surgery and respond well to nonoperative care, such as physiotherapy. Medications may be prescribed by your doctor to help ease pain and muscle spasm. In some cases, the patient's condition is simply monitored to see if symptoms improve.
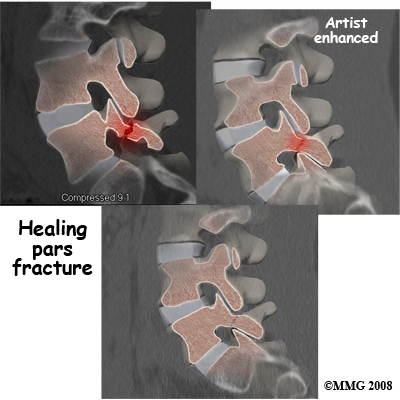
If your doctor diagnoses an acute pars fracture that has the potential to heal, it may be recommended that you wear a rigid back brace for two to three months. This usually occurs in children and teenagers who begin having back pain and see their doctor early on. X-rays may show a fresh fracture of the pars area of the vertebra on one, or both, sides. A CT scan or bone scan may be recommended to determine if the fracture is likely to heal. If so, a brace is recommended. X-rays or a CT scan may be ordered in six to eight weeks to see if the fracture is healing. IF not, the brace will be discontinued.
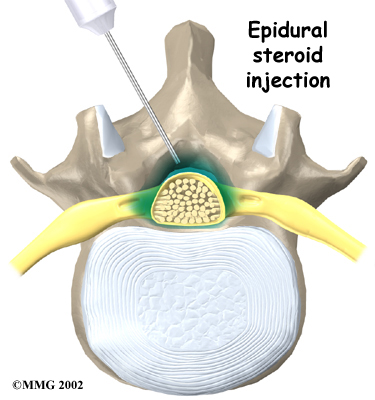
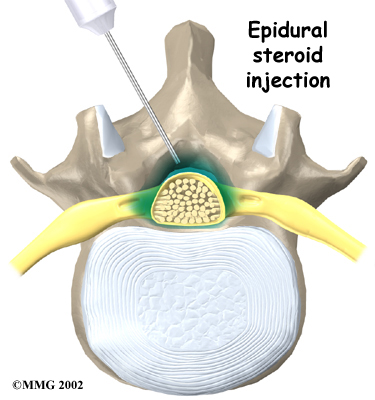
Some patients who continue to have symptoms are given an (ESI). Steroids are powerful anti-inflammatories, meaning they reduce pain and swelling. In an ESI, medication is injected into the space around the lumbar nerve roots. This area is called the epidural space. Some doctors inject only a steroid. Most doctors, however, combine a steroid with a long-lasting numbing medication. Generally, an ESI is given only when other treatments aren't working. But ESIs are not always successful in relieving pain. If they do work, they may only provide temporary relief.
Surgery
Surgery is used when the slip is severe and when symptoms are not relieved with nonsurgical treatments. Symptoms that cause an abnormal walking pattern, changes in bowel or bladder function, or steady worsening in nerve function require surgery. Deterioration of symptoms is common in patients with a history of significant neurologic symptoms who don't have surgery to correct the problem.
 If a reasonable trial of conservative care (three months or more) does not improve things and/or your quality of life is significantly reduced, then surgery may be the next best solution. The main types of surgery for spondylolisthesis include:
If a reasonable trial of conservative care (three months or more) does not improve things and/or your quality of life is significantly reduced, then surgery may be the next best solution. The main types of surgery for spondylolisthesis include:
- laminectomy (decompression)
- posterior fusion with or without instrumentation
- posterior lumbar interbody fusion
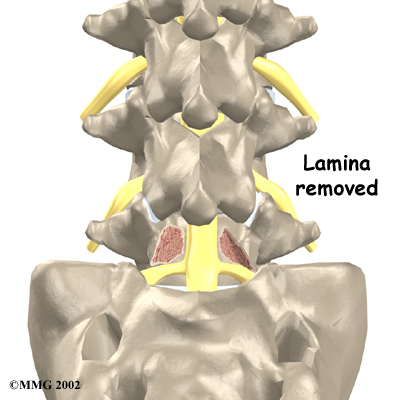
Laminectomy
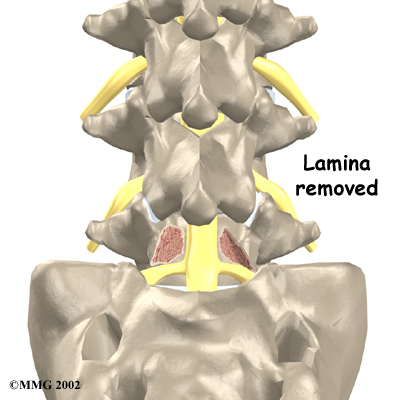
When the vertebra slips forward, the nearby nerves that exit the spine can become pinched or irritated. In addition, the size of the spinal canal in the problem area shrinks, placing pressure on the nerves inside the canal. To fix this, the lamina of the bony ring is removed to ease pressure on the nerves. The procedure to remove the lamina and release pressure on the nerves is called . Decompression alone is usually not advised. Studies show much better results when the operation is combined with a fusion of the involved vertebrae (see below).
Related Document: Kitchener Physiotherapy & Wellness Patient's Guide to Lumbar Laminectomy
Posterior Fusion with Instrumentation
A spinal fusion is normally done immediately after laminectomy for spondylolisthesis. The fusion procedure is designed to fuse the two vertebrae into one bone and stop the slippage from worsening. The fusion is used to lock the vertebrae in place and stop movement between the vertebrae, easing mechanical pain. When combined with laminectomy surgery (mentioned earlier), fusion helps relieve nerve compression.
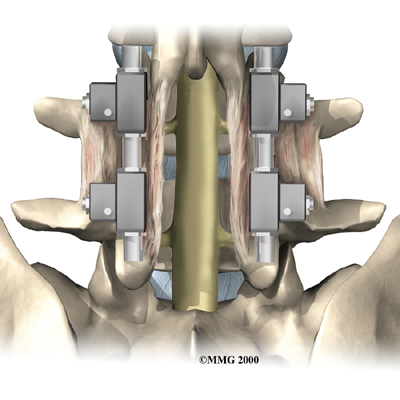
In this procedure, the surgeon lays small grafts of bone over the back of the problem vertebrae. Sometimes fusion is done just with bone graft material. This is a fusion without fixation (non-instrumentation). Instrumentation is the use of metal plates or screws to stabilize the segment during healing. Most surgeons combine fusion with instrumentation to prevent the two vertebrae from moving. This protects the graft so it can heal better and faster.
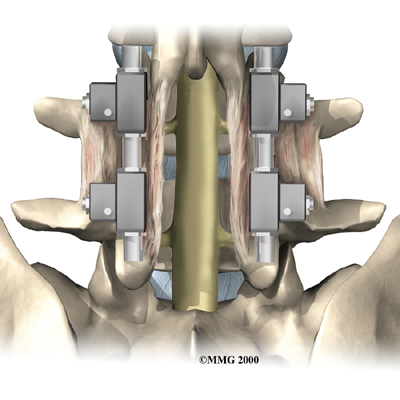
Outcomes are improved when decompression is combined with fusion (compared with decompression alone). Fusion and functional improvement are even better when spinal instrumentation is used. There are fewer long-term problems with pain and pseudoarthrosis (formation of movement or false joints within the fusion).
Related Document: Kitchener Physiotherapy & Wellness to Posterior Lumbar Fusion
Posterior Lumbar Interbody Fusion
When fusion surgery is needed for mild spondylolisthesis (up to 50 percent slippage), posterior lumbar interbody fusion may be considered. In this procedure, the problem vertebrae are fused from the anterior (front) and posterior (back). Combining fusion of both portions of the spine increases the fusion surface area and improves the fusion rate. The surgeon works from the back of the spine and removes the disc between the problem vertebrae. Bone graft material is inserted from the back of the spine into the space between the two vertebrae where the disc was removed (the interbody space). The graft may be held in place with a special fusion cage that spreads and holds the vertebrae apart. Surgeons usually apply some form of instrumentation (described above) on the back of the vertebrae. In some cases, additional strips of bone graft are placed along the back surfaces of the vertebrae to be fused. This increases the mechanical strength of the spine.
Fusion with Biologics
New materials for fusion are being developed and tested. For example, bone morphogenetic proteins (BMP) mixed with bone graft in a putty is under investigation. This substance may help reduce the need for instrumentation with fusion.
BMP helps promote faster and more bone growth in the unstable spinal segment. Studies of safety and effectiveness of this material have been very favorable so far. Without the need to harvest bone graft and place instrumentation, surgical time is much less with BMP putty. And the fusion rate is much higher with BMP alone compared with fusion alone or fusion with fixation.
Motion-Sparing Technologies
The Food and Drug Administration (FDA) is reviewing the use of devices inserted without invasive surgery to limit vertebral motion. For example, a special titanium implant has been designed to fit between the spinous processes of the vertebrae in your lower back.
These motion-sparing devices are currently used with patients who have spinal stenosis (narrowing of the spinal canal or foramen). With spondylolisthesis, the goal is to reduce the load on the disc and facets while increasing the space inside the spinal canal and foramen, thus relieving your symptoms. The vertebral segment is stabilized enough to prevent further progression of the spondylolisthesis.
Portions of this document copyright MMG, LLC.








 Facet joints are small joints that connect the back of the spine together. Normally, the facet joints connecting L5 to the sacrum create a solid buttress to prevent L5 from slipping over the top of the sacrum. However, when problems exist in the disc, facet joints, or bony ring of L5, the buttress becomes ineffective. As a result, the L5 vertebra can slip forward over the top of the sacrum.
Facet joints are small joints that connect the back of the spine together. Normally, the facet joints connecting L5 to the sacrum create a solid buttress to prevent L5 from slipping over the top of the sacrum. However, when problems exist in the disc, facet joints, or bony ring of L5, the buttress becomes ineffective. As a result, the L5 vertebra can slip forward over the top of the sacrum.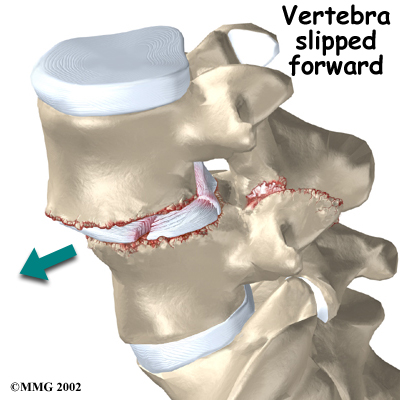
 The pain can be from mechanical causes. Mechanical pain is caused by wear and tear on the parts of the spine. When the vertebra slips forward, it puts a painful strain on the disc and facet joints.
The pain can be from mechanical causes. Mechanical pain is caused by wear and tear on the parts of the spine. When the vertebra slips forward, it puts a painful strain on the disc and facet joints.
 If a reasonable trial of conservative care (three months or more) does not improve things and/or your quality of life is significantly reduced, then surgery may be the next best solution. The main types of surgery for spondylolisthesis include:
If a reasonable trial of conservative care (three months or more) does not improve things and/or your quality of life is significantly reduced, then surgery may be the next best solution. The main types of surgery for spondylolisthesis include: