Introduction
Physiotherapy in Kitchener for Lower Back
Welcome to Kitchener Physiotherapy & Wellness patient resource about Lumbar Disc Herniation.
Although people often refer to a disc herniation as a slipped disc, the disc doesn't actually slip out of place. Rather, the term herniation means that the material at the center of the disc has squeezed out of its normal space. This condition mainly affects people between 30 and 40 years old.
This guide will help you understand:
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the spine are involved?
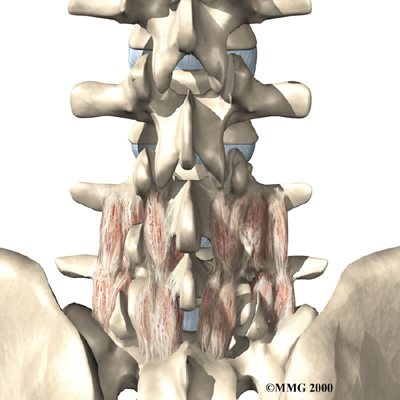
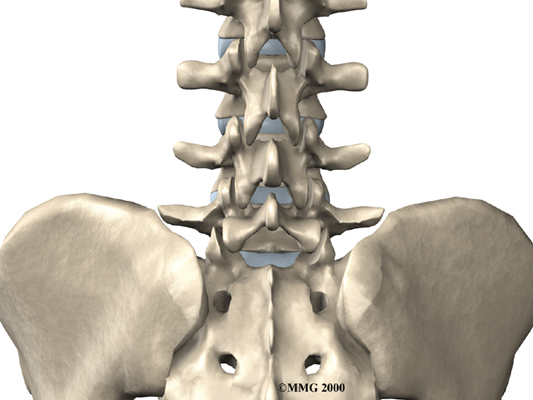
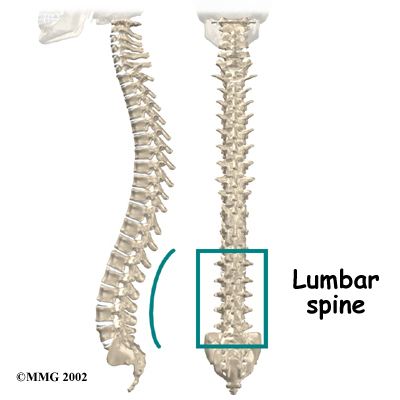
The human spine is formed by 24 spinal bones, called . Vertebrae are stacked on top of one another to form the spinal column. The spinal column gives the body its form. It is the body's main upright support. The section of the spine in the lower back is known as the .
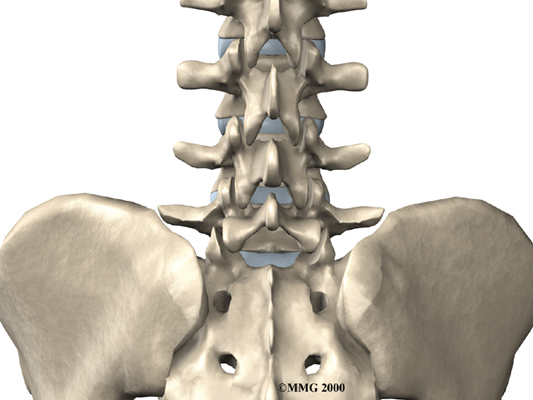
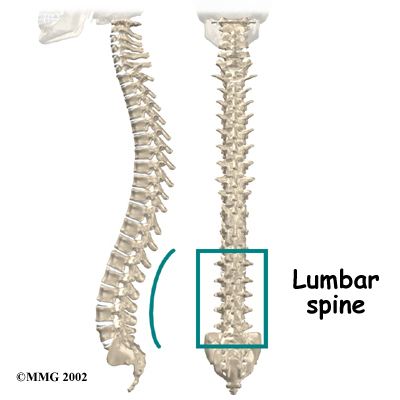
The lumbar spine is made up of the lower five vertebrae. Doctors often refer to these vertebrae as L1 to L5. These five vertebrae line up to give the low back a slight inward curve. The lowest vertebra of the lumbar spine, L5, connects to the top of the sacrum, a triangular bone at the base of the spine that fits between the two pelvic bones. Some people have an extra, or sixth, lumbar vertebra. This condition doesn't usually cause any particular problems.
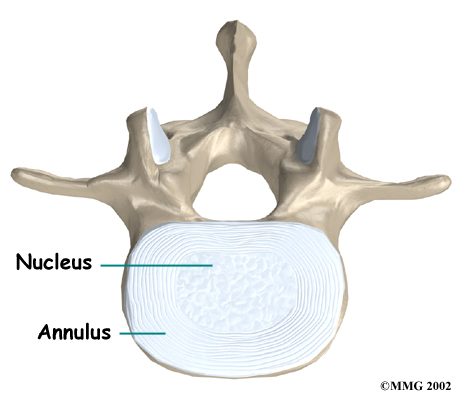
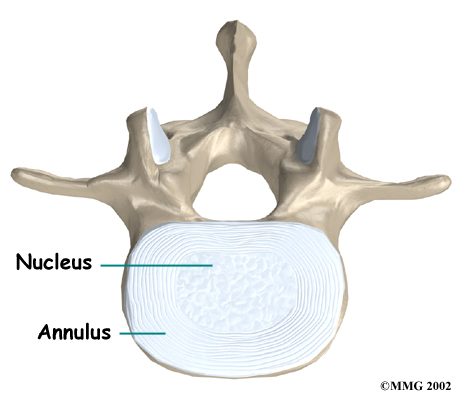 Intervertebral discs separate the vertebrae. The discs are made of connective tissue. Connective tissue is the material that holds the living cells of the body together. Most connective tissue is made of fibers of a material called collagen. These fibers help the disc withstand tension and pressure.
Intervertebral discs separate the vertebrae. The discs are made of connective tissue. Connective tissue is the material that holds the living cells of the body together. Most connective tissue is made of fibers of a material called collagen. These fibers help the disc withstand tension and pressure.
A disc is made of . The center, called the nucleus, is spongy. It provides most of the disc's ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are connective tissues that attach bones to other bones.
Healthy discs work like shock absorbers to cushion the spine. They protect the spine against the daily pull of gravity. They also protect it during strenuous activities that put strong force on the spine, such as jumping, running, and lifting.
Related Document: Kitchener Physiotherapy & Wellness Guide to Lumbar Spine Anatomy
Causes
Why do I have this problem?
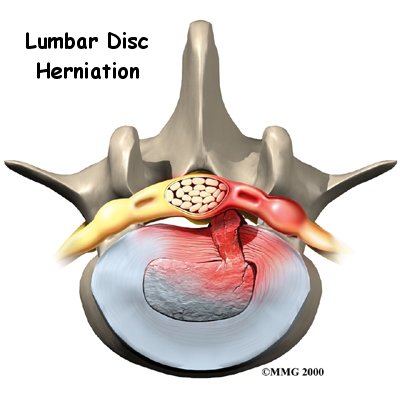
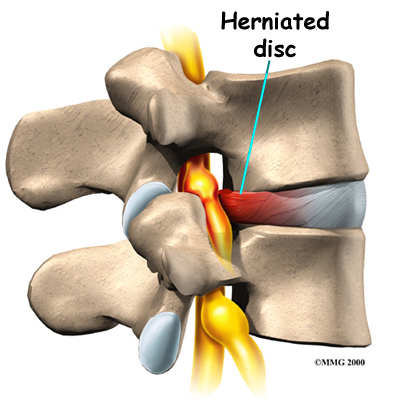
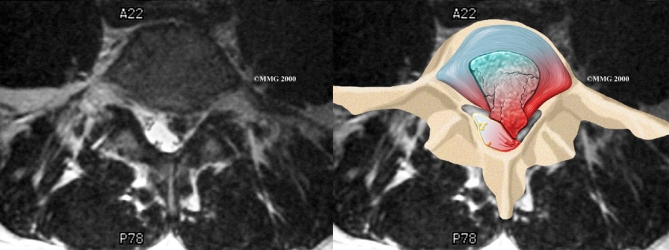
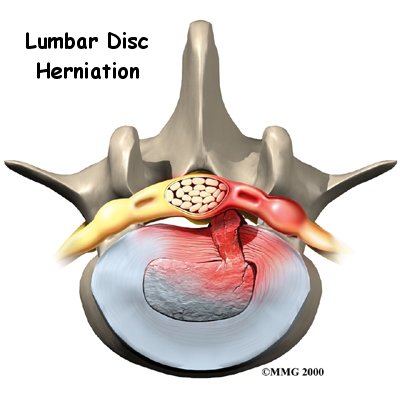
Herniation occurs when the nucleus in the center of the disc pushes out of its normal space. The nucleus presses against the annulus, causing the disc to bulge outward. Sometimes the nucleus herniates completely through the annulus and squeezes out of the disc.
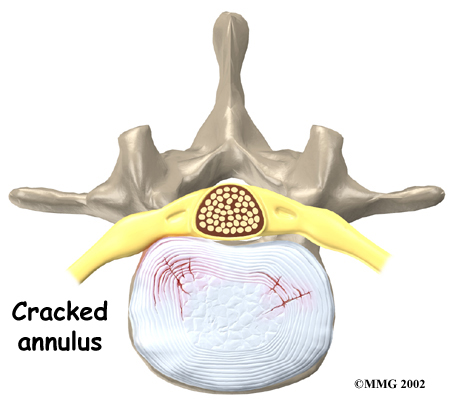 Although daily activities may cause the nucleus to press against the annulus, the body is normally able to withstand this pressure. However, as the annulus ages, it tends to . It is repaired with scar tissue. This process is known as degeneration. Over time, the annulus weakens, and the nucleus may begin to herniate (squeeze) through the damaged annulus. At first, the pressure bulges the annulus outward. Eventually, the nucleus may herniate completely through the outer ring of the disc.
Although daily activities may cause the nucleus to press against the annulus, the body is normally able to withstand this pressure. However, as the annulus ages, it tends to . It is repaired with scar tissue. This process is known as degeneration. Over time, the annulus weakens, and the nucleus may begin to herniate (squeeze) through the damaged annulus. At first, the pressure bulges the annulus outward. Eventually, the nucleus may herniate completely through the outer ring of the disc.
Related Document: Kitchener Physiotherapy & Wellness Guide to Lumbar Degenerative Disc Disease
Vigorous, repetitive bending, twisting, and lifting can place abnormal pressure on the shock-absorbing nucleus of the disc. If great enough, this increased pressure can injure the annulus, leading to herniation.
A lumbar disc can also become herniated during an acute (sudden) injury. Lifting with the trunk bent forward and twisted can cause a disc herniation. A disc can also herniate from a heavy impact on the spine, such as falling from a ladder and landing in a sitting position.
Herniation causes pain from a variety of sources. It can cause mechanical pain. This is pain that comes from the parts of the spine that move during activity, such as the discs and ligaments. Pain from inflammation occurs when the nucleus squeezes through the annulus. The nucleus normally does not come in contact with the body's blood supply. However, a tear in the annulus puts the nucleus at risk for contacting this blood supply. When the nucleus herniates into the torn annulus, the nucleus and blood supply meet, causing a reaction of the chemicals inside the nucleus. This produces inflammation and pain. A disc herniation may also put pressure against a spinal nerve. Pressure on an irritated or damaged nerve can produce pain that radiates along the nerve. This is called neurogenic pain.
Symptoms
 Many cases of lumbar disc herniation result from degenerative changes in the spine. The changes that eventually lead to a disc herniation produce symptoms gradually. At first, complaints may only be dull pain centered in the low back, pain that comes and goes over a period of a few years. Doctors think this is mainly from small tears in the annulus. Larger cracks in the annulus may spread pain into the buttocks or lower limbs.
Many cases of lumbar disc herniation result from degenerative changes in the spine. The changes that eventually lead to a disc herniation produce symptoms gradually. At first, complaints may only be dull pain centered in the low back, pain that comes and goes over a period of a few years. Doctors think this is mainly from small tears in the annulus. Larger cracks in the annulus may spread pain into the buttocks or lower limbs.
When the disc herniates completely through the annulus, it generally causes immediate symptoms, with sharp pain that starts in one hip and shoots down part or all of the leg. Commonly, patients no longer feel their usual back pain, only leg pain. This is likely because painful tension on the annulus releases when the nucleus pushes completely through.
Disc herniations produce inflammation when the nucleus comes in contact with the body's blood supply (mentioned earlier). The inflammation can be a source of throbbing pain in the low back and may spread into one or both hips and buttocks.
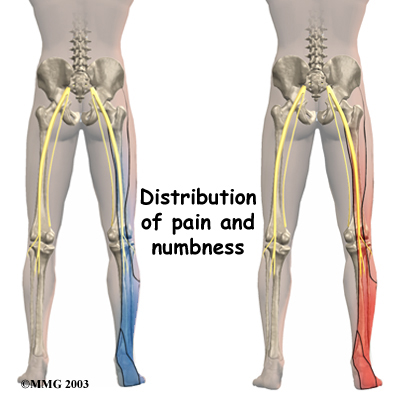
A herniated disc can press against a spinal nerve, producing symptoms of nerve compression. Nerve pain follows . It can be felt on the side of the upper thigh, in the calf, or even in the foot and toes.
Pressure on the nerve can also cause sensations of where the nerve travels down the lower limbs. If this happens, a person's reflexes slow. The muscles controlled by the nerve weaken, and sensation in the skin where the nerve goes is impaired.
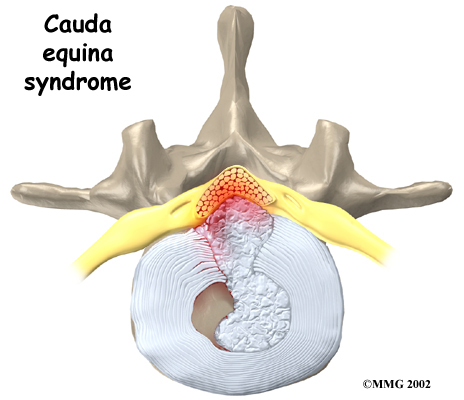
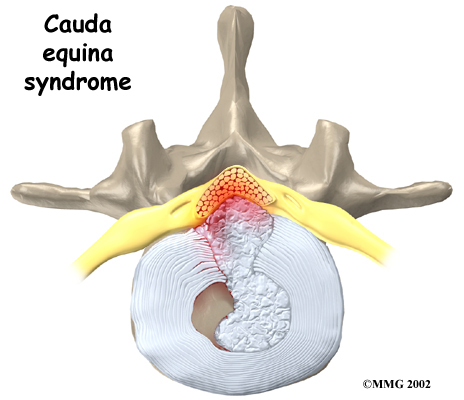
Rarely, symptoms involve changes in bowel and bladder function. A large disc herniation that pushes straight back into the spinal canal can put pressure on the nerves that go to the bowels and bladder. The pressure may cause low back pain, pain running down the back of both legs, and numbness or tingling between the legs in the area you would contact if you were seated on a saddle. The pressure on the nerves can cause a loss of control in the bowels or bladder. This is an emergency. If the pressure isn't relieved, it can lead to permanent paralysis of the bowels and bladder. This condition is called . Doctors recommend immediate surgery to remove pressure from the nerves.
Diagnosis
How do health care providers diagnose the problem?
Diagnosis begins with a complete history and physical exam. When you first visit Kitchener Physiotherapy & Wellness, we will ask questions about your symptoms and how your problem is affecting your daily activities. These will include questions about where you feel pain and whether you have numbness or weakness in your legs. Our physiotherapist will also want to know what positions or activities make your symptoms worse or better. We rely on your report of pain to get an idea about which disc is causing problems and if a nerve is being squeezed.
Then our physiotherapist will physically examine you to determine which back movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are also tested.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physiotherapists at Kitchener Physiotherapy & Wellness have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Our Treatment
Non-surgical Rehabilitation
Unless your condition is causing significant problems or is rapidly getting worse, treatment for lumbar disc herniation usually begins with nonsurgical treatment. Most people with a herniated lumbar disc get better without surgery. As a result, it is usually recommended that patients try nonoperative treatments for at least six weeks before considering surgery.
At first, your physiotherapist at Kitchener Physiotherapy & Wellness may want your low back immobilized. Keeping the back still for a short time can calm inflammation and pain. This might include a period of bed rest. Lying on your back can take pressure off sore discs and nerves. However, our physiotherapists usually advise against strict bed rest and prefer their patients to do ordinary activities using pain to gauge how much is too much. In rare cases in which bed rest is prescribed, it is usually used for a maximum of two days.
A back support belt is sometimes used for patients with lumbar disc herniation. The belt can help lower pressure inside the problem disc. Our patients are encouraged to gradually discontinue wearing the support belt over a period of two to four days. Otherwise, their trunk muscles begin to rely on the belt and start to weaken and atrophy (shrink).
Our physiotherapy treatments focus on relieving pain, improving back movement, and fostering healthy posture. The first goal of our treatment is to control symptoms. Your physiotherapist will help you find positions and movements that ease pain. Treatments of heat, cold, ultrasound, and electrical stimulation may be used in the first few sessions. Lumbar traction may also be used at first to ease symptoms of lumbar disc herniation. In addition, our physiotherapist may use hands-on treatments such as massage or spinal manipulation. These forms of treatment are mainly used to help reduce pain and inflammation so you can resume normal activity as soon as possible.
Your physiotherapist will show you how to keep your spine safe during routine activities. You'll learn about healthy posture and how posture relates to the future health of your spine. We will teach you about body mechanics, how the body moves and functions during activity. Our physiotherapists teach safe body mechanics to help you protect the low back as you go about your day. This includes the use of safe positions and movements while lifting and carrying, standing and walking, and performing work duties.
The next part of our program will include a series of strengthening exercises for the abdominal and low back muscles. Working these core muscles helps our patients begin moving easier and lessens the chances of future pain and problems. Aerobic exercises such as walking or swimming are used for easing pain and improving endurance.
We will work closely with your doctor and employer to help you get back on the job as quickly as reasonably possible. You may be required to do lighter duties at first, but as soon as you are able, you'll begin doing your normal work activities. Our therapist can do a work assessment to make sure you'll be safe to do your job. We may suggest changes that could help you work safely, with less chance of re-injuring your back.
A primary purpose of your physiotherapy is to help you learn how to take care of your symptoms yourself and prevent future problems. We'll provide you with a home program of exercises to continue improving flexibility, posture, endurance, and low back and abdominal strength. Our physiotherapist will also discuss strategies you can use if your symptoms flare up.
When patients simply aren't getting better during their therapy program, or if the problem is becoming more severe, surgery may be suggested.
Post-surgical Rehabilitation
Rehabilitation after surgery is more complex. Some patients leave the hospital shortly after surgery. However, some surgeries require patients to stay in the hospital for a few days.
During recovery from surgery, patients should follow their surgeon's instructions about wearing a back brace or support belt, and should be cautious about overdoing activities in the first few weeks after surgery.
Although recovery time varies for each patient, as a guideline you may expect to see our therapist for one to three months, depending on the type of surgery. At first, your physiotherapists may use treatments such as heat or ice, electrical stimulation, massage, and ultrasound to help calm pain and muscle spasm. We provide reassurance to help you deal with fear and apprehension about pain. Then our therapist will teach you how to move safely while putting the least strain on your healing back. Exercises are used to improve flexibility, strength, and endurance.
When your recovery is well under way, your regular visits to Kitchener Physiotherapy & Wellness will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Physician Review
are of minor help in diagnosing disc herniations. The discs don't actually show up on X-rays. However, doctors can tell if the space between the vertebrae is smaller than normal. This can be an indication that wear and tear on one or more discs is causing problems. However, many peoples' X-rays show degeneration of the discs. This is because degeneration in the discs is part of aging, like skin that wrinkles with time.

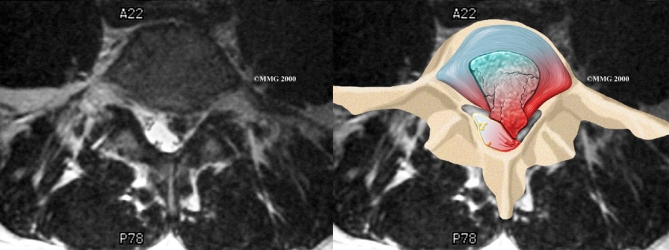
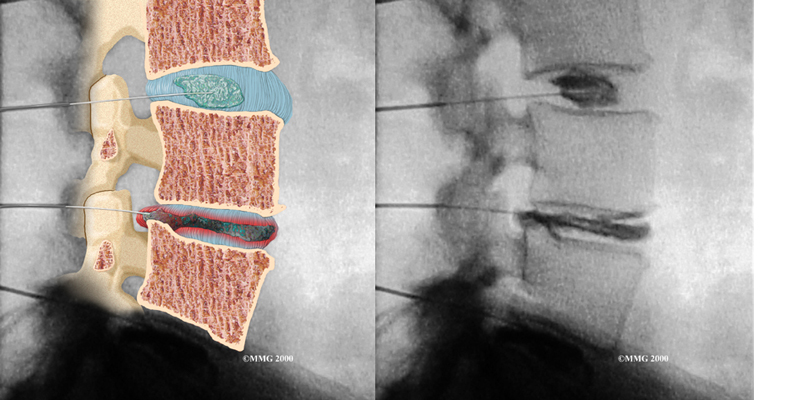
Computed tomography (a CT scan) may be ordered. This is a detailed X-ray that lets doctors see slices of the body's tissue. The image can show if a herniated disc is putting pressure on a spinal nerve.
Doctors may combine the CT scan with myelography. To do this, a special dye is injected into the space around the spinal canal, called the the subarachnoid space. When the CT scan is performed, the dye highlights the spinal cord and nerves. The dye can improve the accuracy of a standard CT scan for diagnosing a herniated disc.
When more information is needed, your doctor may order (MRI). The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. It gives a clear picture of the discs and whether a herniation is present. Like the CT scan, this machine creates pictures that look like slices of the area your doctor is interested in. The test does not require special dye or a needle.
Doctors sometimes order a specialized X-ray test called . In this test, dye is injected into one or more discs. The dye is seen on X-ray and can give some information about the health of one or more discs. This test may be used when surgery is being considered to determine which disc is causing problems.
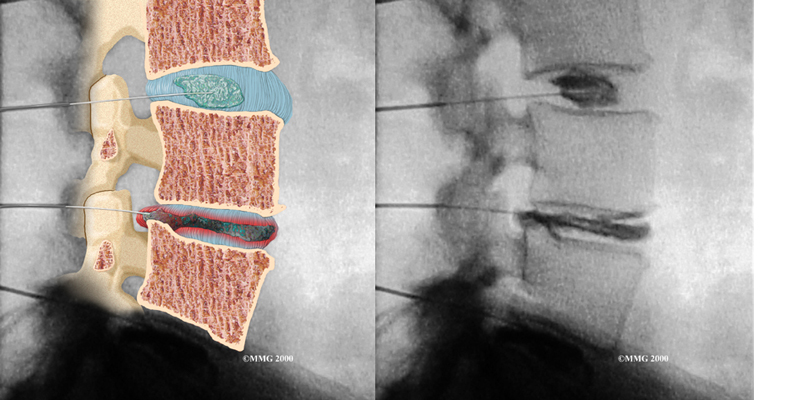
Doctors may also order electrical tests to locate more precisely which spinal nerve is being squeezed. Several tests are available to see how well the nerves are functioning, including the electromyography (EMG) test. This test measures how long it takes a muscle to work once a nerve signals it to move. The time it takes will be slower if a herniated disc has put pressure on a spinal nerve. Another test is the somatosensory evoked potential (SSEP) test. The SSEP is used to measure nerve sensations. These sensory impulses travel up the nerve, informing the body about sensations such as pain, temperature, and touch. The function of a nerve is recorded by an electrode placed over the skin in the area where the nerve travels. Doctors will often run these tests before performing surgery for a lumbar disc herniation.
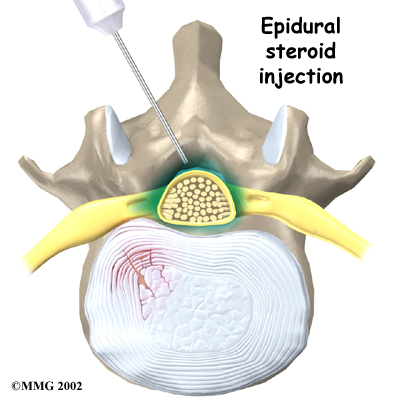
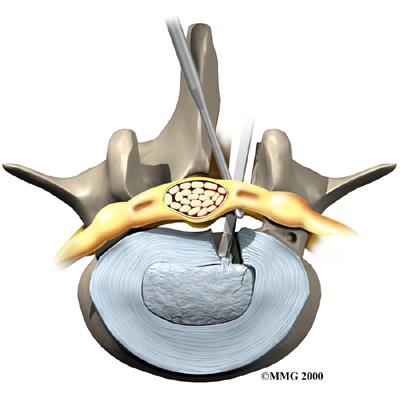
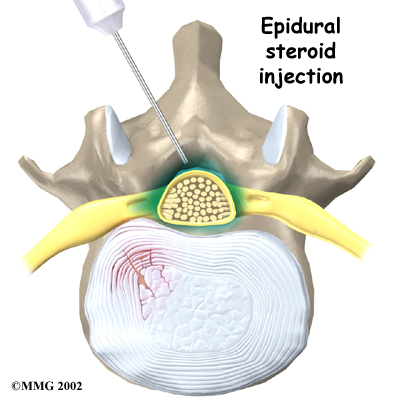
Some patients who continue to have symptoms are given an (ESI). Steroids are powerful anti-inflammatories. In an ESI, medication is injected into the space around the lumbar spinal nerves where they branch off of the spinal cord. This area is called the epidural space. Some doctors inject only a steroid. Most doctors, however, combine a steroid with a long-lasting numbing medication. Generally, an ESI is given only when other treatments aren't working. But ESIs are not always successful in relieving pain. If they do work, they often provide only temporary relief.
Surgery
If the symptoms you feel are mild and there is no danger they'll get worse, surgery is not usually recommended. However, if signs appear that pressure is building on the spinal nerves, surgery may be required, sometimes right away. The signs doctors watch for when reaching this decision include weakening in the leg muscles, pain that won't ease up, and problems with the bowels or bladder.
Surgical treatment for lumbar disc herniation includes:
- laminotomy and discectomy
- microdiscectomy
- posterior lumbar fusion
Laminotomy and Discectomy
The lamina forms a roof-like structure over the back of the spinal canal. In this procedure, a thumbnail-sized piece of the lamina is removed (laminotomy) so the surgeon can more easily take out the problem disc (discectomy). This procedure is mainly used when the herniated disc is putting pressure on a nerve and causing pain to spread down one leg.
Related Document: Kitchener Physiotherapy & Wellness Guide to Lumbar Discectomy
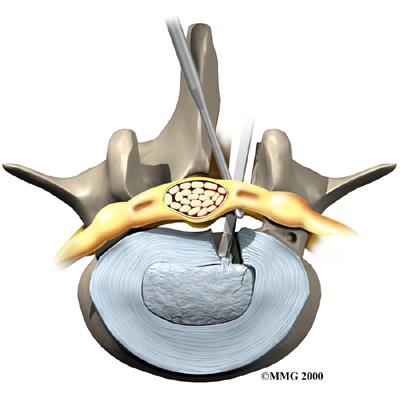
Microdiscectomy
Microdiscectomy is becoming the standard surgery for lumbar disc herniation. The procedure is used when a herniated disc is putting pressure on a nerve root. It involves carefully taking out part of the problem disc (discectomy). By performing the operation with a surgical microscope, the surgeon only needs to make a very small incision in the low back. Categorized as minimally invasive surgery, this surgery is thought to be less taxing on patients. Advocates also believe that this type of surgery is easier to perform, that it prevents scarring around the nerves and joints, and that it helps patients recover more quickly.
Related Document: Kitchener Physiotherapy & Wellness Guide to Lumbar Discectomy
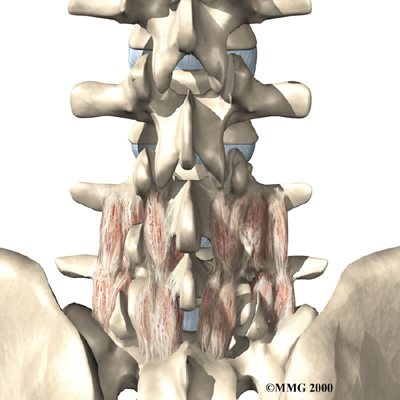
 Posterior Lumbar Fusion
Posterior Lumbar Fusion
Lumbar disc herniation causes mechanical pain, the type of pain caused by wear and tear in the parts of the lumbar spine. Fusion surgery is mainly used to stop movement of the painful area by joining two or more vertebrae into one solid bone. This keeps the bones and joints from moving, easing mechanical pain.
In posterior lumbar fusion, the surgeon over the problem area on the back of the spinal column. Most surgeons will also apply metal plates and screws to prevent the problem vertebrae from moving. This protects the graft so it can heal better and faster.
Related Document: Kitchener Physiotherapy & Wellness Guide to Posterior Lumbar Fusion
Portions of this document copyright MMG, LLC.








 Intervertebral discs separate the vertebrae. The discs are made of connective tissue. Connective tissue is the material that holds the living cells of the body together. Most connective tissue is made of fibers of a material called collagen. These fibers help the disc withstand tension and pressure.
Intervertebral discs separate the vertebrae. The discs are made of connective tissue. Connective tissue is the material that holds the living cells of the body together. Most connective tissue is made of fibers of a material called collagen. These fibers help the disc withstand tension and pressure.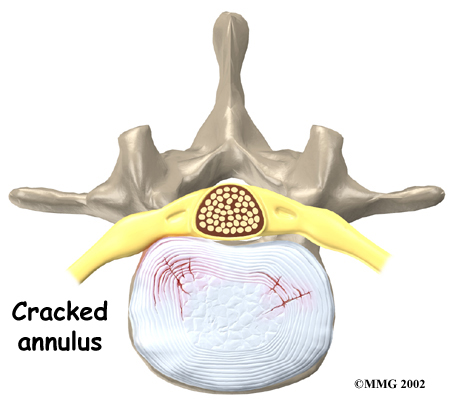 Although daily activities may cause the nucleus to press against the annulus, the body is normally able to withstand this pressure. However, as the annulus ages, it tends to
Although daily activities may cause the nucleus to press against the annulus, the body is normally able to withstand this pressure. However, as the annulus ages, it tends to 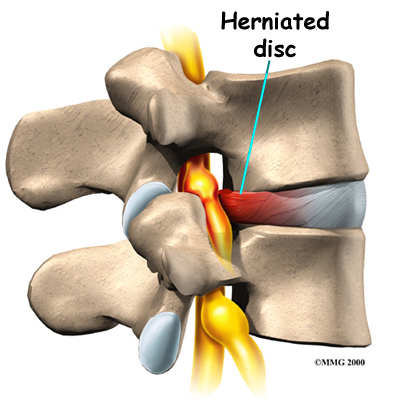
 Many cases of lumbar disc herniation result from degenerative changes in the spine. The changes that eventually lead to a disc herniation produce symptoms gradually. At first, complaints may only be dull pain centered in the low back, pain that comes and goes over a period of a few years. Doctors think this is mainly from small tears in the annulus. Larger cracks in the annulus may spread pain into the buttocks or lower limbs.
Many cases of lumbar disc herniation result from degenerative changes in the spine. The changes that eventually lead to a disc herniation produce symptoms gradually. At first, complaints may only be dull pain centered in the low back, pain that comes and goes over a period of a few years. Doctors think this is mainly from small tears in the annulus. Larger cracks in the annulus may spread pain into the buttocks or lower limbs.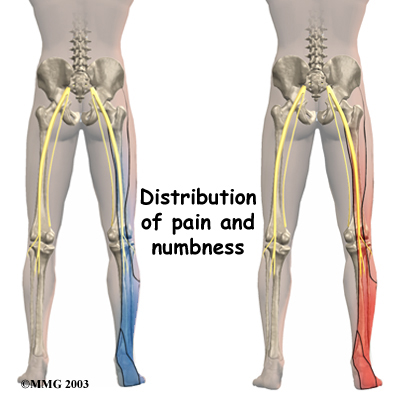

 Posterior Lumbar Fusion
Posterior Lumbar Fusion