Introduction
Physiotherapy in Kitchener for Hand Issues
Welcome to Kitchener Physiotherapy & Wellness resource on resection arthroplasty.
 Thumb arthritis may be surgically treated with a procedure called resection arthroplasty or sometimes called excision arthroplasty. The term excision means to take out. In this surgery, the surgeon takes out a small bone at the base of the thumb and fills in the space with a rolled up section of tendon. The soft tissue forms a false joint that keeps the thumb somewhat mobile and stops pain by preventing the joint surfaces from rubbing together.
Thumb arthritis may be surgically treated with a procedure called resection arthroplasty or sometimes called excision arthroplasty. The term excision means to take out. In this surgery, the surgeon takes out a small bone at the base of the thumb and fills in the space with a rolled up section of tendon. The soft tissue forms a false joint that keeps the thumb somewhat mobile and stops pain by preventing the joint surfaces from rubbing together.
This guide will help you understand:
- which parts of the thumb are involved
- why this type of surgery is used
- what happens during the procedure
- what to expect before and after surgery
- what Kitchener Physiotherapy & Wellness approach to rehabilitation is
Anatomy
Which parts of the thumb are involved?
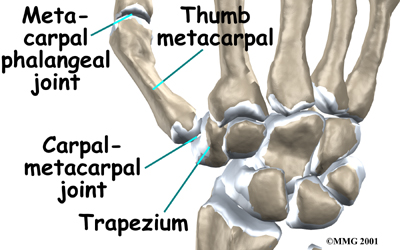
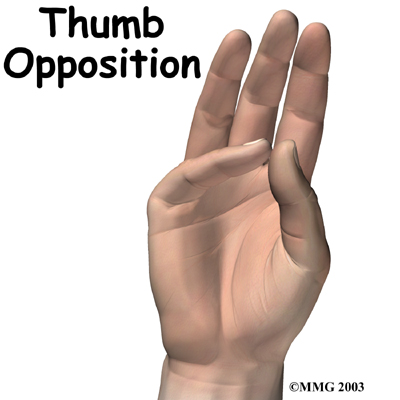
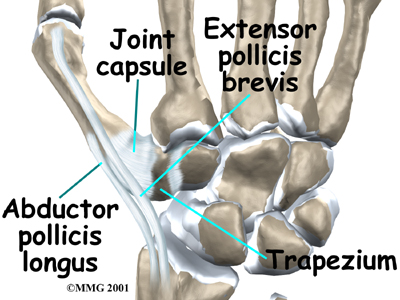
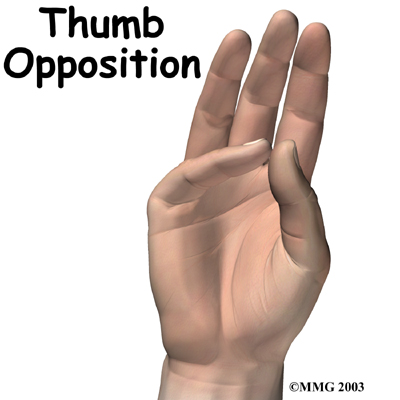
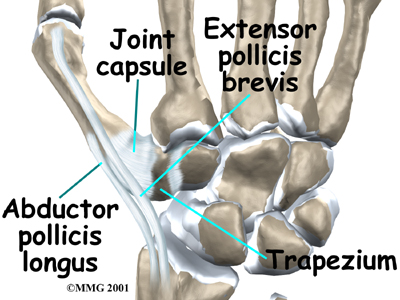
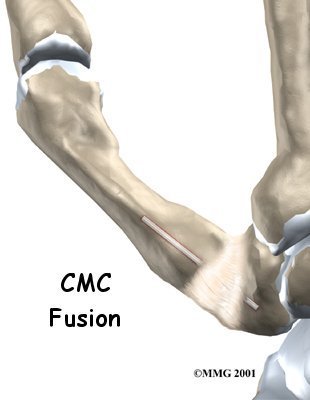
The carpometacarpal joint (or CMC joint) of the thumb is where the metacarpal bone of the thumb attaches to the trapezium bone of the wrist. This joint is sometimes referred to as the basal joint of the thumb. The CMC joint is the one that allows you to move your thumb into your palm, a motion called opposition.
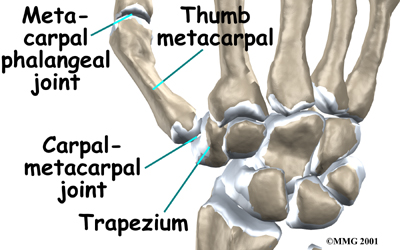
Several ligaments (strong bands of tissue) hold the joint together. These ligaments join to form the joint capsule of the CMC joint. The joint capsule is a watertight sac around the joint.
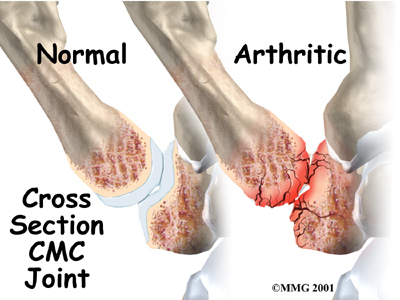
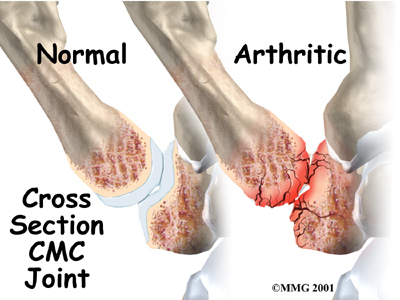
The joint surfaces are covered with a material called articular cartilage. This material is the slick, spongy covering that allows one side of a joint to slide against the other joint surface easily. When this material wears out, the joint develops a type of arthritis called osteoarthritis and becomes painful.
Rationale
What does the surgeon hope to achieve?
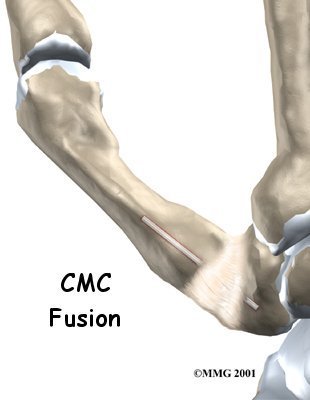
The main goal of this surgery is to ease pain where the surfaces of the thumb joint are rubbing together. The surgeon uses a piece of tendon to form a spacer that separates the surfaces of the CMC joint. Unlike a fusion surgery that simply binds the joint together, excision arthroplasty can help take away pain while allowing the thumb joint to retain some movement.
Rationale
What should I do to prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps to ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn't eat or drink anything after midnight the night before.
Surgical Procedure
What happens during surgery?
 Surgery can last up to 90 minutes. Surgery may be done using a general anesthetic, which puts you completely to sleep, or a local anesthetic, which numbs only the hand. With a local anesthetic you may be awake during the surgery, but you won't be able to see the surgery.
Surgery can last up to 90 minutes. Surgery may be done using a general anesthetic, which puts you completely to sleep, or a local anesthetic, which numbs only the hand. With a local anesthetic you may be awake during the surgery, but you won't be able to see the surgery.
Once you have anesthesia, your surgeon will make sure the skin of your hand is free of infection by cleaning the skin with a germ-killing solution. An incision will be made which angles along the back of the thumb to the edge of the wrist. Special care is taken not to damage the nearby nerve going to the thumb.
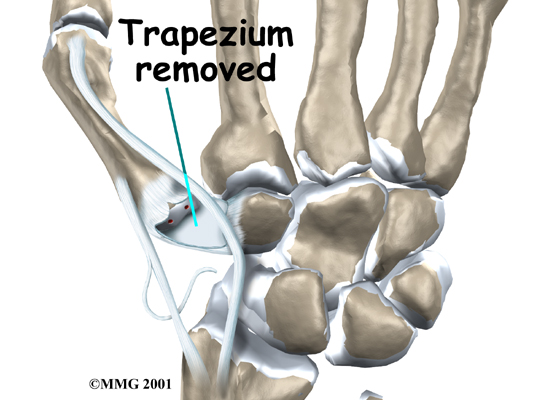
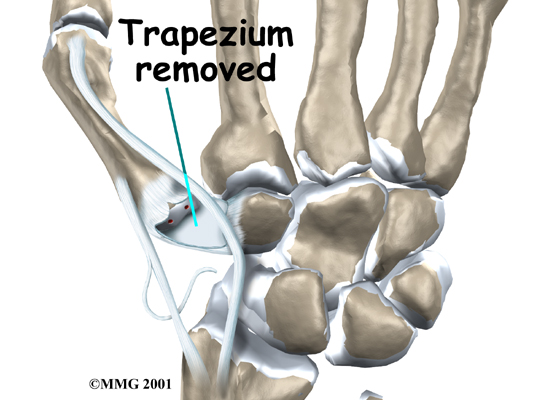
The CMC joint and surrounding tissues are exposed. Next, the joint capsule surrounding the CMC joint is opened. The surgeon takes out (excises) the trapezium bone at the base of the thumb.
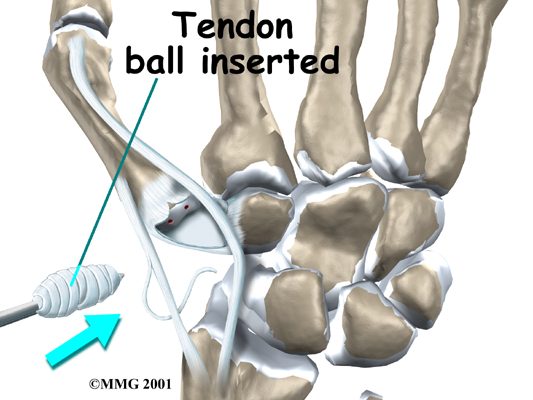
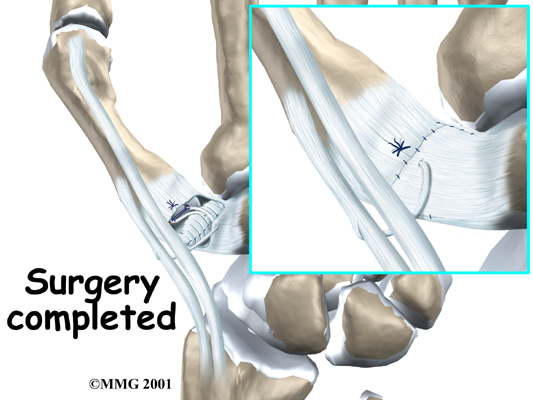
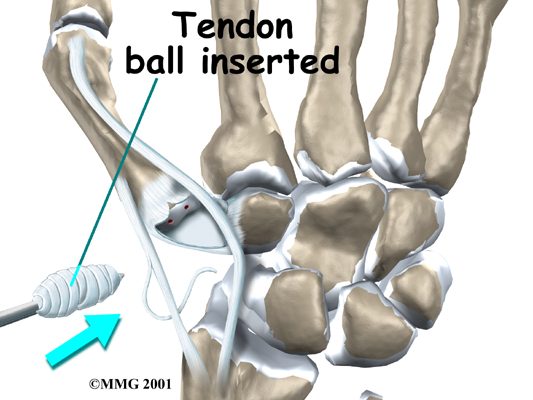
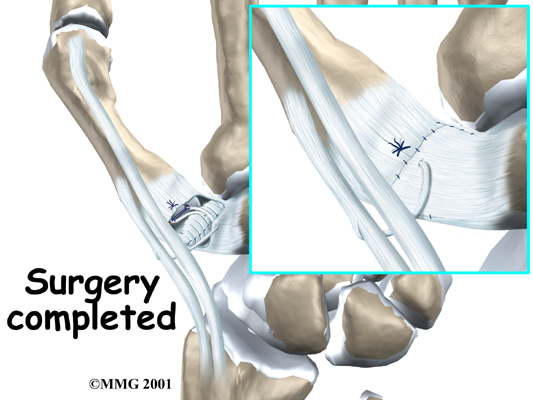
Next the surgeon removes a small section of one of the tendons near the thumb. The piece of tendon is sewn into a small ball and placed into the space where the trapezium bone was removed. The remaining portion of the tendon is sewn to the thumb metacarpal to stabilize the joint. The surgeon may also insert a surgical pin to connect and hold the metacarpal bones of the thumb and index finger. The pin protects the reconstructed joint and is usually removed three weeks after the surgery.
The soft tissues over the joint are sewn back together. The thumb is placed in a splint, and the hand is wrapped in a bulky dressing.
After Surgery
What happens after surgery?
After surgery, your thumb will be bandaged with a well-padded dressing and a splint for support. The splint will keep the thumb in a natural position during healing. You will be required to wear a thumb brace for up to six weeks to give the repair time to heal. Your surgeon will want to check your hand within five to seven days. Stitches will be removed after 10 to 14 days, though most of your stitches will be absorbed into your body. If a surgical pin was used, it will be removed three weeks after surgery.
You should keep your hand elevated above the level of your heart for several days to avoid swelling and throbbing. Keep it propped up on a stack of pillows when sleeping or sitting up.
You may have some discomfort after excision arthroplasty. You will be given pain medicine to control the discomfort.
Rehabilitation
What should I expect during my recovery period?
Physiotherapy treatment at Kitchener Physiotherapy & Wellness can begin as soon as you are no longer required to wear your thumb brace, and once your surgeon has given approval for you to begin your rehabilitation. If some minimal support for your thumb continues to be required after wearing the rigid brace your physiotherapist may tape your thumb or prescribe a small soft flexible brace that you can wear as needed while you begin your rehabilitation.
Your initial few physiotherapy treatments will focus on relieving any lingering pain associated with the surgical process as well as the period of immobilization. Your physiotherapist may use modalities such as heat, ice, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the surgical site or anywhere into your hand or along your arm. Massage to these areas may also be done in order to improve circulation and assist with the pain.
The next part of treatment will focus on regaining the range of motion, strength, and dexterity in your thumb, wrist, hand, elbow, and even shoulder. Your physiotherapist at Kitchener Physiotherapy & Wellness will prescribe a series of range of motion and strengthening exercises that you will practice in the clinic and also learn to do as part of your home exercise program. Full motion of your thumb, including opposition, as well as motions enabling your thumb to extend fully away from your palm will be encouraged. The prescribed range of motion and strength exercises may include the use of rehabilitation equipment such as mini pulleys, putty, elastics or balls for strengthening and gripping resistance. In addition to strengthening your grip we will educate you on ways to grip and support items in order to do your tasks without putting too much stress on your new thumb joint.
If necessary, your physiotherapist will mobilize your thumb joint or any other joint in the area that is stiff and impeding normal movement of your hand and limb. This hands-on technique encourages the stiff joints to move gradually into their normal range of motion.
Minimizing or eliminating your pain as well as being able to move your hand and thumb so that you can complete your work tasks and daily activities is the goal of our therapy at Kitchener Physiotherapy & Wellness. Maximizing dexterity of your thumb and its fine motor abilities post surgically can greatly improve the functional use of your hand. For this reason, we will also incorporate specific activities into your rehabilitation program like picking up items from a table or twisting items into place using your surgical hand. Other exercises might include activities that are specific to the tasks you personally need to complete on a regular daily basis, such as typing or picking up papers or dishes. These functional activities encourage the joints and the muscles of the hand and arm to work in unison, which is critical to maximizing the use of your entire upper limb. Exercises where weight is put through your new joint, such as pressing the pad of your thumb into different surfaces, will also be added when the thumb is ready. These exercises encourage your surgical joint to tolerate weight in a controlled fashion. Finally, your physiotherapist will discuss ways that you can modify some of your regular activities in order to decrease the overall stress put on your thumb and to avoid problems with your thumb and hand in the future.
When you are well underway, regular visits to Kitchener Physiotherapy & Wellness will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program. In most cases you will need to attend regular therapy sessions for one to two months, but you should expect full recovery to take up to four months. Ongoing tissue remodeling will occur even up to 12 months post-surgery.
In the majority of cases the physiotherapy we provide at Kitchener Physiotherapy & Wellness after resection arthroplasty of the thumb occurs without any complications. If, however, during rehabilitation your pain continues longer than it should or therapy is not progressing as your physiotherapist would expect, we will ask you to follow-up with your surgeon to confirm that the joint is tolerating the rehabilitation well and to ensure that there are no hardware issues that may be impeding your recovery.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Complications
What might go wrong due to surgery?
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following resection arthroplasty are:
- anesthesia problems
- infection
- nerve damage
Anesthesia
Problems can arise when the anesthesia given during surgery, which causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Any operation carries a small risk of infection. Resection arthroplasty of the thumb is no different. You will probably be given antibiotics before the operation to reduce the risk of infection. If an infection occurs you will most likely need antibiotics to cure it. You may need additional operations to drain the infection if it involves the area around the arthroplasty.
Nerve Damage
All of the nerves and blood vessels that go to the thumb travel across, or near, the CMC joint. Being that the operation is performed so close to these important structures, it is possible to injure either the nerves or the blood vessels during surgery. The result may only be temporary if the damage has been caused due to the nerve being stretched by surgical retractors, which hold the nerves out of the way. It is uncommon to have permanent injury to either the nerves or the blood vessels, but it is possible.
Portions of this document copyright MMG, LLC
 Thumb arthritis may be surgically treated with a procedure called resection arthroplasty or sometimes called excision arthroplasty. The term excision means to take out. In this surgery, the surgeon takes out a small bone at the base of the thumb and fills in the space with a rolled up section of tendon. The soft tissue forms a false joint that keeps the thumb somewhat mobile and stops pain by preventing the joint surfaces from rubbing together.
Thumb arthritis may be surgically treated with a procedure called resection arthroplasty or sometimes called excision arthroplasty. The term excision means to take out. In this surgery, the surgeon takes out a small bone at the base of the thumb and fills in the space with a rolled up section of tendon. The soft tissue forms a false joint that keeps the thumb somewhat mobile and stops pain by preventing the joint surfaces from rubbing together.